Higher LDL-c variability associated with lower cognitive function
08/08/2016
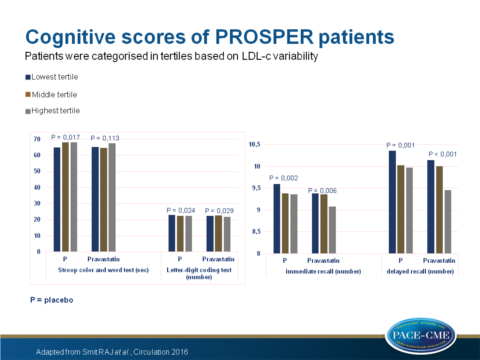
In elderly PROSPER study patients at high CV risk, a high variability of LDL-c levels was associated with lower cognitive scores, based on 4 cognitive tests.
Higher Visit-to-Visit Low-Density Lipoprotein Cholesterol Variability Is Associated With Lower Cognitive Performance, Lower Cerebral Blood Flow, and Greater White Matter Hyperintensity Load in Older SubjectsLiterature - Smit RAJ et al., Circulation 2016
Smit RAJ, Trompet S, Sabayan B, et al.
Circulation 2016;134:212-221
Background
It has recently been shown that LDL-c variability is associated with risk of coronary and other cardiovascular events, stroke and mortality, independent of mean LDL-c levels: greater visit-to-visit variability is associated with a higher risk of experiencing these events (1). It is unknown whether this variability also associates with cognitive performance.Hereto, 4428 participants enrolled in the PROSPER (PROspective Study of Pravastatin in the Elderly at Risk) study were analysed, and fasting visit-to-visit LDL-c variability and its association with cognitive function was assessed. Furthermore, the link with LDL-c variability and hippocampal volume, cerebral blood flow and white matter hyperintensity load was examined in a magnetic resonance imaging (MRI) substudy (n = 535).
In the PROSPER study, patients were treated with pravastatin and LDL-c levels were measured at 0, 3, 6, 12 and 24 months after follow-up, however baseline measurements were excluded from the analysis. After 30 months, cognitive outcome was evaluated through 4 cognitive measures: immediate and delayed recall (Picture-word learning test), the ‘Stroop colour and word test’, and the ‘Letter-digit coding test’.
Main results
- Pravastatin reduced both average LDL-c levels (-1.18 mmol/L, 95%CI: -1.14 tot -1.22) as mean visit-to-visit LDL-c variability (-0.02 mmol/L, 95%CI: -0.01 tot -0.04).
- After full model adjustment, higher LDL-c variability was associated with lower cognitive scores in lowest vs. middle vs. highest LDL-c variability tertile, regarding immediate recall (placebo: 9.60, 9.38, 9.36 counts, P trend = 0.002 and pravastatin: 9.38, 9.36, 9.08 counts, P trend = 0.006); delayed recall (placebo: 10.36, 10.03, 9.97 counts, P trend = 0.001 and pravastatin: 10.14, 10.00, 9.46 counts, P trend < 0.001); Stroop test (placebo: 65.06, 68.00, 68.00 seconds, P trend = 0.017 and pravastatin: 65.17, 64.70, 67.54 seconds, P trend = 0.11); Letter-digit coding test (placebo: 23.05, 22.29, 22.39 counts, P trend = 0.20 and pravastatin: 22.41, 22.81, 21.72 counts, P trend = 0.029).
- No interaction was observed between LDL-c variability and pravastatin treatment for the cognitive outcomes.
- LDL-c variability was not associated with hippocampal volume.
- After full model adjustment, higher LDL-c variability was associated with lower total cerebral blood flow in the placebo group (46.95, 47.21, 44.12 ml/min/100ml, P trend = 0.031) and pravastatin group (48.80, 49.89, 47.33 ml/min/100ml, P trend = 0.050), with a greater white matter hyperintensity load in the pravastatin group (4.50, 6.88, 8.43 ml, P trend = 0.046) but not placebo group.
Download Smit Circulation 2016 PACE.pptx
 Conclusion
Conclusion
Higher visit-to-visit LDL-c variability was associated with lower cognitive performance, lower cerebral blood flow and greater white matter hyperintensity load in older participants at risk for vascular disease. This suggests that LDL-c is a useful prognostic marker for different clinical outcomes.Find this article online at Circulation
References
1. Bangalore S, Breazna A, DeMicco DA, et al; TNT Steering Committee and Investigators. Visit-to-visit lowdensity lipoprotein cholesterol variability and risk of cardiovascular outcomes: insights from the TNT trial. J Am Coll Cardiol. 2015;65:1539–1548. doi: 10.1016/j.jacc.2015.02.017.
