Inflammation in End-Stage Renal Disease
The purpose of this review is to summarize the main advances contributing to our current understanding of the complex inflammatory processes present in ESRD....
Inflammation in End-Stage Renal Disease—What Have We Learned in 10 Years?Literature - Juan J. Carrero and Peter Stenvinkel; Seminars in Dialysis—Vol 23, No 5 (September–October) 2010 pp. 498–509
Juan J. Carrero and Peter Stenvinkel
Seminars in Dialysis—Vol 23, No 5 (September–October) 2010 pp. 498–509
The first reports connecting uremic inflammation with a wasted and atherogenic phenotype and poor outcome initiated in the late 1990s. Since then, about 3500 publications appear on Medline, reflecting the exponential interest that this topic has evoked in nephrology. What was described as a ‘‘novel’’ risk factor 10 years ago has now evolved into an established finding in patients with end-stage renal disease (ESRD). The purpose of this review is to summarize the main advances contributing to our current understanding of the complex inflammatory processes present in ESRD. Causes and consequences of inflammation, genetic heritability of the inflammatory response, implications on outcome prognostication, and contemporary therapeutic evidence are some of the various topics discussed.
Inflammation and end-stage renal disease (ESRD) are already an old and intimately related couple. Apart from a hypotheses presented in the mid 1980s linking exposure of whole blood to cellulosic membranes with increased IL-1 production as a cause of hemodialysis (HD) hypotension (1), it was not until the late 1990s that the first reports on uremic inflammation and its relation
to cardiovascular disease (CVD), protein-energy wasting (PEW) (2), and worse outcome (3–6) were presented.
What was at that time described as a ‘‘novel’’ risk factor (7) has by now evolved into an established risk factor in patients with CKD. During the last decade, there has been much progress in elucidating the molecular mechanisms that lead to inflammatory reactions (8). Moreover, we have also learnt a lot concerning the characteristic inflammatory profile of uremic patients, which results from both retention of inflammatorymediators and increased tissue production. The purpose of this review is to summarize
the main advances occurred with regard to the understanding of the complex inflammatory processes in ESRD.
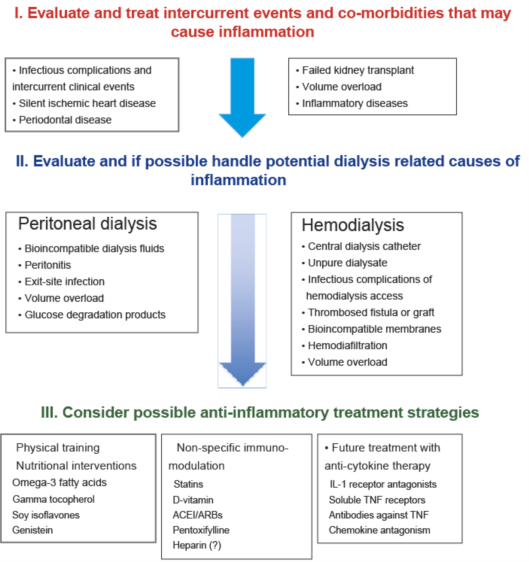
Suggested steps to target persistent inflammation in dialysis patients.
Summary & Conclusion
The authors summarized that much has been learnt during the last decade about the flabbergastingly complex inflammatory interactions that exist in patients with advanced CKD. However, intervention trials have not yet been initiated to prove the concept that persistent inflammation is not only a driver of many features commonly observed in uremia (such as wasting, depression, accelerated atherosclerosis, or vascular calcification) but also a causalmortality risk factor.Given the natural variability of inflammation biomarkers in the context of uremia, such intervention studies will require large study populations and extensive funding. It is our hope that when we revisit the status of knowledge with regard to uremic inflammation in ten years time,many of these issues would have been tackled and, optimistically, solved.
References
1. Henderson IS, Koch KM, Dinarello CA, Shaldon S: Hemodialysis hypotension:the interleukin hypothesis. Blood Purif 1:3–8, 1983
2. Stenvinkel P, Heimburger O, Paultre F, Diczfalusy U, Wang T, Berglund L, Jogestrand T: Strong association between malnutrition, inflammation, and atherosclerosis in chronic renal failure. Kidney Int 55:1899–1911, 1999
3. Zimmermann J, Herrlinger S, Pruy A, Metzger T, Wanner C: Inflammation enhances cardiovascular risk and mortality in hemodialysis patients. Kidney Int 55:648–658, 1999
4. Iseki K, Tozawa M, Yoshi S, Fukiyama K: Serum C-reactive (CRP) and risk of death in chronic dialysis patients. Nephrol Dial Transplant 14:1956–1960, 1999
5. Noh H, Lee SW, Kang SW, Shin SK, Choi KH, Lee HY, Han DS: Serum C-reactive protein: a predictor ofmortality in continuous ambulatory peritoneal dialysis patients.NephrolDial Transplant 18:387–394, 1998
6. BologaRM, LevineDM, Parker TS,Cheigh JS, SerurD, StenzelKH, Rubin AL: Interleukin-6 predicts hypoalbuminemia, hypocholesterolemia,andmortality in hemodialysis patients.AmJ KidneyDis 32:107–114, 1998
7. Stenvinkel P, Alvestrand A: Inflammation in end-stage renal disease:sources, consequences, and therapy. SeminDial 15:329–337, 2002