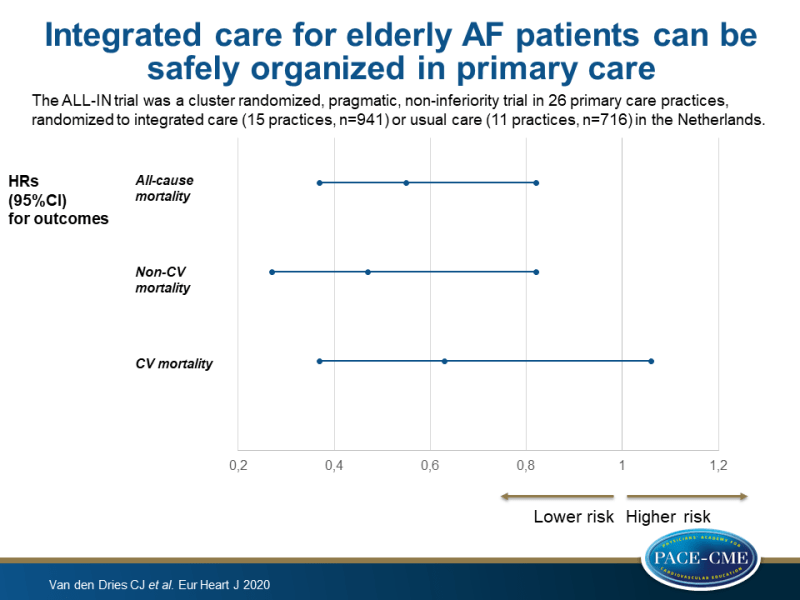
Integrated care for elderly AF patients can be safely organized in primary care
This cluster randomized, non-inferiority trial showed that integrated care for elderly AF patients in a primary care setting led to a 45% reduction in all-cause mortality compared with usual care.
Integrated management of atrial fibrillation in primary care: results of the ALL-IN cluster randomized trialLiterature - Van den Dries CJ et al., - Eur Heart J. 2020. pii: ehaa055. doi: 10.1093/eurheartj/ehaa055.
Introduction and methods
Atrial fibrillation (AF) is no longer merely viewed as an isolated heart rhythm disorder with an increased risk of stroke, but more as a ‘hypercoagulable state’ which can be associated with multiple underlying and interacting comorbidities [1]. Integrated care that includes the management of comorbidities could address the increasing disease burden of AF and is recommended in the 2016 ESC guidelines on the management of AF (Class IIa recommendation, level of evidence B) [2].
A meta-analysis showed that integrated care coordinated by tertiary care hospitals led to a reduction in all-cause mortality and CV hospitalization [3]. Furthermore, the RACE 4 trial showed that integrated, nurse-led care in experienced AF clinics led to reduced cardiac mortality and hospitalization [4]. However, it remains unknown whether integrated care can be safely organized in a primary care setting, which is characterized by non-specialist doctors and nurses and AF patients that are typically older, frailer and more often suffer from multimorbidity. This study investigated whether integrated care can be safely organized in primary care.
The ALL-IN trial was a cluster randomized, pragmatic, non-inferiority trial in primary care in the Netherlands. 26 Primary care practices were randomized to the intervention arm (15 practices, n=941 patients, aged ≥65 years, were included) or usual care arm (11 practices, n=716 patients, aged ≥65 years, were included). The intervention consisted of three components: (i) quarterly check-ups by the practice nurse on symptoms and comorbidities, assessment of early signs and symptoms of heart failure, and patient education, (ii) management of anticoagulant treatment, such as INR measurements performed by the intervention practice in patients on a vitamin K antagonist (VKA), attention to drug compliance, and monitoring of kidney function in patients using a non-vitamin K antagonist oral anticoagulant (NOAC), and (iii) consultation with anticoagulation clinics and/or cardiologists, enabling shared care and responsibility. Usual care varied between patients, but most often involved a once yearly visit to a cardiologist or AF nurse at an outpatient cardiology department.
All practices completed at least 2 years of follow-up. The median follow-up was 2.3 years in the intervention arm and 2.2 years in the control arm. The primary outcome was all-cause mortality. Secondary outcomes were CV and non-CV mortality, CV and non-CV hospitalization, MACE, stroke, major bleeding, clinically relevant non-major bleeding, and health-related quality of life.
Main results
- Patients in the intervention arm showed a 45% reduction in all-cause mortality compared with patients in the usual care arm (adjusted HR 0.55, 95%CI 0.37-0.82).
- Risk reductions of CV mortality and non-CV mortality were observed in the intervention arm compared with usual care, and risk reduction of non-CV mortality was more pronounced than risk reduction of CV mortality (adjusted HR for non-CV mortality 0.47, 95%CI 0.27-0.82; and adjusted HR for CV mortality 0.63, 95%CI 0.37-1.06).
- Patients in the intervention arm showed a 16% reduction of all-cause hospitalization (adjusted IRR 0.84, 95%CI 0.69-1.03), with a similar effect for CV hospitalization (adjusted IRR 0.86, 95%CI 0.60-1.22) and non-CV hospitalization (adjusted IRR 0.83, 95%CI 0.66-1.05).
- No statistically significant differences were found for secondary outcomes MACE, ischemic stroke, major bleeding, and clinically relevant non-major bleeding. Changes in health-related quality of life were minimal in both groups.
Conclusion
This trial evaluated whether integrated care for AF in elderly patients can be safely organized in primary care. Integrated care involved quarterly check-ups by a practice nurse, anticoagulation monitoring and easy-access collaboration between healthcare professionals. Integrated care for elderly AF patients led to a 45% reduction in all-cause mortality compared with usual care in the Netherlands.
References
1. Van Doorn S, Tavenier A, Rutten FH, Hoes AW, Moons KGM, Geersing GJ. Risk of cardiac and non-cardiac adverse events in community-dwelling older patients with atrial fibrillation: a prospective cohort study in the Netherlands. BMJ Open 2018;8:1–7.
2. Kirchhof P, Benussi S, Kotecha D et al., 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J 2016;37:2893–2962.
3. Gallagher C, Elliott AD, Wong CX, Rangnekar G, Middeldorp ME, Mahajan R, Lau DH, Sanders P, Hendriks J. Integrated care in atrial fibrillation: a systematic review and meta-analysis. Heart 2017:1–7.
4. Wijtvliet EPJP, Tieleman RG, van Gelder IC, Pluymaekers NAHA, Rienstra M, Folkeringa RJ, Bronzwaer P, Elvan A, Elders J, Tukkie R, Luermans JGLM, Van Asselt A, Van Kuijk SMJ, Tijssen JG, Crijns HJGM; RACE 4 Investigators. Nurse-led vs. usual-care for atrial fibrillation. Eur Heart J 2020;41:634–641.
