Intensive lipid lowering reduces CV morbidity and CHD death in resistant hypertension
In the TNT trial, atorvastatin 80 mg significantly decreased the risk of the primary outcome in patients with treatment-resistant hypertension, as compared with atorvastatin 10 mg.
Lipid lowering in patients with treatment-resistant hypertension: an analysis from the Treating to New Targets (TNT) trialLiterature - Bangalore S et al., Eur Heart J. 2014 - Eur Heart J. 2014 Jul 14;35(27):1801-8
Bangalore S, Fayyad R, Laskey R, et al; Treating to New Targets Steering Committee and Investigators
Eur Heart J. 2014 Jul 14;35(27):1801-8
Background
Hypertension is an important modifiable risk factor. Although much progress has been made in the control of hypertension, a substantial part of patients still has treatment-resistant hypertension (TRH: defined by the American Heart Association as blood pressure (BP) that remains above goal despite concurrent use of 3 antihypertensive agents of different classes) [1-3]. Patients with TRH have an increased risk of cardiovascular (CV) events [1,4,5].New therapeutic approaches using ablation of sympathetic neural activity or stimulating carotid baroreceptors are being tested, with the aim to reduce BP in this high-risk population. None of these trials have been powered to show a significant reduction in the risk of CV events.
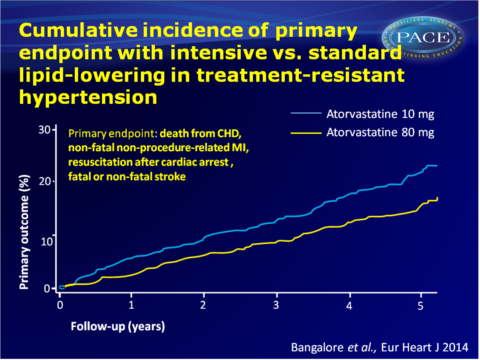
The effect of lipid lowering on CV outcomes is unknown in these high-risk subpopulations. This study therefore evaluated the effect of intensive lipid lowering on the risk of CV outcomes in patients with TRH. This was part of the double-blind Treating to New Targets (TNT) Study [6,7], in which patients with coronary artery disease (CAD), were randomised to atorvastatin 80 vs. 10 mg. 1112 patients in the TNT trial had TRH, of whom 388 (35%) patients achieved systolic BP goal of <140 mmHg with four or more antihypertensive agents. The primary endpoint was occurrence of death from coronary heart disease (CHD), non-fatal non-procedure-related myocardial infarction, resuscitation after cardiac arrest, or fatal or non-fatal stroke at the end of follow-up (up to 5 years).
Main results
- No significant difference in reduction in BP from baseline was seen between the two atorvastatin dosing groups.
- Similar to the results of the main trial, significant reductions in LDL-c, non-HDL-c, total cholesterol and triglycerides were seen in patients on atorvastatin 80 mg as compared with atorvastatin 10 mg. At the last follow-up moment, LDL-c was 20.8 mg/dL lower in the atorvastatin 80 mg group (mean 78.6 vs. 99.4 mg/dL, P<0.001). This difference was relatively steady from 3 months onwards.
- Atorvastatin 80 mg was associated with a 30% lower risk of the primary endpoint than atorvastatin 10 mg (14.5 vs. 19.9%, P=0.01), which was mainly the result of a 45% reduction in CHD deaths. No difference was seen in the incidence of stroke (4.0 vs. 4.7%, P=0.53).
- A dose of 80 mg was also associated with 33% lower risk of a major coronary event, 17% reduction in any CV event, and 23% reduction in any coronary event, as compared to 10 mg.
- No differences in the occurrence of treatment-emergent adverse events (AEs), nor discontinuation due to AEs or myalgia were seen between atorvastatin 80 vs. 10 mg. Elevation in hepatic enzymes was rare in both groups, but more frequent in the 80 mg group, although no patients had CPK elevation >10x ULN in either group.
Download Bangalore EHJ 2014 PACE.pptx
Conclusion
Patients with treatment-resistant hypertension showed a significantly lower risk of the primary outcome after intensive lipid-lowering therapy with atorvastatin 80 mg, mostly driven by fewer CHD deaths. Although BP reduction in TRH is very important to reduce the long-term risk of CV and cerebrovascular events, this non-BP reducing strategy can also yield a considerable reduction in the risk of CV morbidity and mortality in this high-risk population.Find this article on Pubmed
References
1. Daugherty SL, Powers JD, Magid DJ, et al. Incidence and prognosis of resistant hypertension in hypertensive patients. Circulation 2012;125:1635–1642.
2. Egan BM, Zhao Y, Axon RN, et al. Uncontrolled and apparent treatment resistant hypertension in the United States, 1988 to 2008. Circulation 2011;124:1046–1058.
3. Persell SD. Prevalence of resistant hypertension in the United States, 2003–2008. Hypertension 2011;57:1076–1080.
4. Pierdomenico SD, Lapenna D, Bucci A, et al. Cardiovascular outcome in treated hypertensive patients with responder, masked, false resistant, and true resistant hypertension. Am J Hypertens 2005;18:1422–1428.
5. Symplicity HTNI, Esler MD, Krum H, et al. Renal sympathetic denervation in patients with treatment-resistant hypertension (The Symplicity HTN-2 Trial): a randomised controlled trial. Lancet 2010; 376:1903–1909.
6. Waters DD, Guyton JR, Herrington DM, et al. Treating to New Targets (TNT) Study: does lowering low-density lipoprotein cholesterol levels below currently recommended guidelines yield incremental clinical benefit? Am J Cardiol 2004;93:154–158.
7. LaRosa JC, Grundy SM, Waters DD, et al. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med 2005;352:1425–1435.
