Intraarterial treatment within 6 hours after stroke onset improves functional recovery
18/12/2014
MR CLEAN study shows that intraarterial thrombolysis and/or thrombectomy at a proximal intracranial occlusion of the anterior circulation is safe and effective in patients with acute ischaemic stroke.
BackgroundLiterature - Berkhemer OA et al., NEJM 2014
A Randomized Trial of Intraarterial Treatment for Acute Ischemic Stroke
Berkhemer OA, Fransen PS, Beumer D et al; the MR CLEAN Investigators
N Engl J Med. 2014 Dec 17. [Epub ahead of print]
The only reperfusion therapy in patients with acute ischaemic stroke with proven efficacy is intravenous alteplase, if administered within 4.5 hours after symptom onset [1]. Its therapeutic time window is, however, narrow and several contraindications prevent its use in some [2]. Furthermore, it is not as effective at opening proximal occlusions of the major intracranial arteries, which are a common cause of acute stroke [3,4]. Recanalisation after alteplase is seen in only about one third of patients with an occluded internal-carotid artery terminus [5]. Without revascularisation, prognosis is generally poor [6].
In addition to locally delivered thrombolytic agents, intraarterial therapy can be applied by thrombectomy with mechanical devices. Contradicting results and suboptimal study designs have resulted in uncertainty regarding the efficacy of the catheter-based approach [7-9].
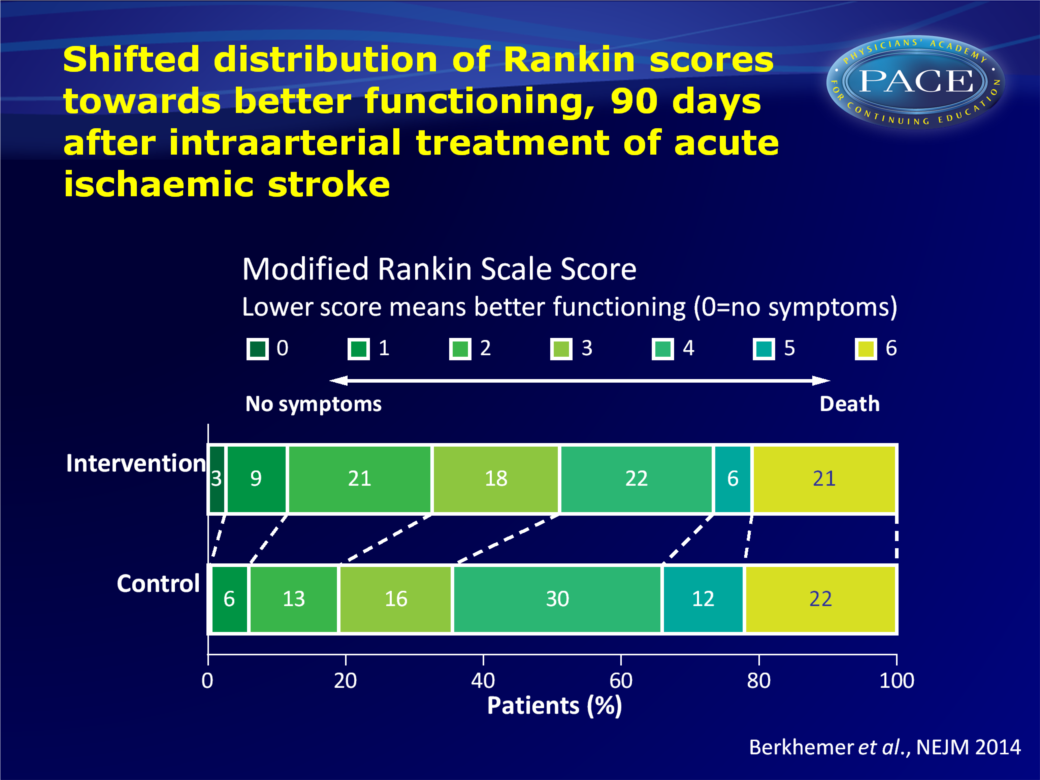
MR CLEAN (The Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands) assessed whether interaarterial treatment plus usual care was more effective than usual care alone in patients with a proximal arterial occlusion in the anterior cerebral circulation, if treated intra-arterially within 6 hours after symptom onset. In a pragmatic, phase 3, multicenter clinical trial set up, MR CLEAN addressed previous methodological limitations. Open-label treatment was randomised, but end-point evaluation was blinded. Intraarterial treatment consisted of arterial catheterisation with a microcatheter to the level of occlusion to perform mechanical thrombectomy or deliver a thrombolytic agent, or both (choice of method was left to discretion of interventionist). 500 patients participated in the study. The primary outcome was the score on the modified Rankin scale at 90 days.
Main results
- A shift was seen in the distribution of the modified Rankin scale scores in favour of the intervention, consistent in all categories of the scale, except for death (adjusted common OR: 1.67, 95%CI: 1.21-2.30).
- 13.5% (95%CI: 5.9-21.2) more patients were functionally independent (modified Ranking score 0-2) after the intervention, than in the control group (32.6% vs. 19.1%, adjusted OR: 2.16, 95%CI: 1.39-3.38).
- The intervention positively influenced all clinical and imaging secondary outcomes, the NIHSS score after 5-7 days was for instance on average 2.9 points (95%CI: 1.5-4.3) lower than in the control group.
- Absence of residual occlusion at the target site, as assessed by CTA after 24 hours, was more common in the intervention group (141/187 patients (75.4%) vs. 68/207 (32.9%).
- Infarct volume was smaller after the intervention, with a between-group difference of 19 ml (95%CI: 3-34).
- No difference was seen between the two treatment groups in the frequency of serious adverse events during the 90 days of follow-up. No difference in mortality was seen at 7, 30 or 90 days. More (13/233, 5.6%) patients in the intervention group showed clinical signs of a new ischaemic stroke in a different vascular territory within 90 days than in the control group (1/267, 0.4%).
- The observed effect was consistent across all predefined subgroups.
Conclusion
Functional recovery in patients with acute ischaemic stroke caused by a proximal intracranial arterial occlusion of the anterior circulation is better after intraarterial treatment, if administered within 6 hours after stroke onset. In 82% of cases, retrievable stents were used. The fact that these positive findings contradict earlier neutral efficacy results for intraarterial treatment may stem from the requirement in MR CLEAN of a radiologically proven intracranial occlusion for study elegibility.Find this article on Pubmed
References
1. Emberson J, Lees KR, Lyden P, et al. Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischaemic stroke: a meta-analysis of indi- vidual patient data from randomised tri- als. Lancet 2014 August 5 (Epub ahead of print).2. Jauch EC, Saver JL, Adams HP Jr, et al. Guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/ American Stroke Association. Stroke 2013;44:870-947.
3. Beumer D, Saiedie G, Fonvile S, et al. Intra-arterial occlusion in acute ischemic stroke: relative frequency in an unselected population.CerebrovascDis2013;35:Suppl: 66.
4. Heldner MR, Zubler C, Mattle HP, et al. National Institutes of Health Stroke Scale score and vessel occlusion in 2152 patients with acute ischemic stroke. Stroke 2013; 44:1153-7.
5. Christou I, Burgin WS, Alexandrov AV, Grotta JC. Arterial status after intrave- nous TPA therapy for ischaemic stroke: a need for further interventions. Int Angiol 2001;20:208-13.
6. Lima FO, Furie KL, Silva GS, et al. Prognosis of untreated strokes due to an- terior circulation proximal intracranial arterial occlusions detected by use of computed tomography angiography. JAMA Neurol 2014;71:151-7.
7 Broderick JP, Palesch YY, Demchuk AM, et al. Endovascular therapy after in- travenous t-PA versus t-PA alone for stroke. N Engl J Med 2013;368:893-903. [Erratum, N Engl J Med 2013;368:1265.]
8. Ciccone A, Valvassori L, Nichelatti M, et al. Endovascular treatment for acute ischemic stroke. N Engl J Med 2013;368: 904-13.
9. Kidwell CS, Jahan R, Gornbein J, et al. A trial of imaging selection and endovas- cular treatment for ischemic stroke. N Engl J Med 2013;368:914-23.
