Lipoprotein risk factors in cardiovascular disease prediction
25/06/2012
Risk prediction scores for cardiovascular disease (CVD) contain information on total cholesterol, HDL-C and several other conventional risk factors. Whether CVD prediction could be improved by assessing various additional lipid-related markers to replace or to supplement traditional cholesterol measurements was evaluated in this study.
Lipid-related markers and cardiovascular disease predictionLiterature - The Emerging Risk Factors Collaboration, JAMA 2012; June 20, 307:2499-2506
The Emerging Risk Factors Collaboration
JAMA 2012, June 20;307:2499-2506
Risk prediction scores for cardiovascular disease (CVD) contain information on total cholesterol, HDL-C and several other conventional risk factors [1,2]. Whether CVD prediction could be improved by assessing various additional lipid-related markers to replace or to supplement traditional cholesterol measurements is an interesting topic [3].
Aims of this study were to determine whether replacing information on total cholesterol and HDL-C with various lipid parameters improves prediction of first-onset CVD outcomes, and secondly to determine whether additional information on apolipoprotein B and A-I, lipoprotein(a), or lipoprotein-associated phospholipase A2 to prognostic models containing information on total cholesterol, HDL-C, and other conventional risk factors improves CVD risk prediction.
Data on 165 000 individuals from 37 cohort studies where these apolipoproteins were measured at baseline were combined and the patients were followed for an average of 10 years.
The additional apolipoproteins do not add much to risk prediction over routine lipid measures. The main reason for this is probably that cardiovascular disease is multifactorial and that apolipoproteins are only one set of factors among many. A common mistake in clinical practice is to overly emphasize one or another risk factor as a predictive factor. This is particularly problematic when risk factors are colinearly linked, as occurs between lipid and apolipoprotein risk factors. The predictive power of various biomarkers does not necessarily equate to the benefit achieved by reducing them. So epidemiological studies cannot be taken as the final word, and drug therapy that targets the risk factor might still prove more efficacious than would be predicted from epidemiological studies.
Recommendations for statin use in primary prevention may need to be revisited now anyway, and risk assessment may in the future move away from measuring many biomarkers and instead focus on subclinical atherosclerosis with imaging methods or simple risk projection based on age, sex, LDL levels, and perhaps another major risk factor.
1. Perk J, De Backer G, Gohlke H, et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012): The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts) [published online May 2, 2012]. Eur Heart J
2. Parish S, Offer A, Clarke R, et al. Lipids and Lipoproteins and Risk of Different Vascular Events in the MRC/BHF Heart Protection Study. Circulation. 2012;125(20):2469-2478
3. Arsenault BJ, Boekholdt SM, Kastelein JJP. Lipid parameters for measuring risk of cardiovascular disease. Nat Rev Cardiol. 2011;8(4):197-206
4. Grundy S M. Use of emerging lipoprotein risk factors in assessment of cardiovascular risk. JAMA 2012; 307:2540-2542.
Context
The value of assessing various emerging lipid-related markers for prediction of first cardiovascular events is debated.
Objective To determine whether adding information on apolipoprotein B and apolipoprotein A-I, lipoprotein(a), or lipoprotein-associated phospholipase A2 to total cholesterol and high-density lipoprotein cholesterol (HDL-C) improves cardiovascular disease (CVD) risk prediction.
Design, Setting, and Participants
Individual records were available for 165 544 participants without baseline CVD in 37 prospective cohorts (calendar years of recruitment: 1968-2007) with up to 15 126 incident fatal or nonfatal CVD outcomes (10 132 CHD and 4994 stroke outcomes) during a median follow-up of 10.4 years (interquartile range, 7.6-14 years).
Main Outcome Measures
Discrimination of CVD outcomes and reclassification of participants across predicted 10-year risk categories of low (<10%), intermediate (10%-<20%), and high (≥20%) risk.
Results
The addition of information on various lipid-related markers to total cholesterol, HDL-C, and other conventional risk factors yielded improvement in the model's discrimination: C-index change, 0.0006 (95% CI, 0.0002-0.0009) for the combination of apolipoprotein B and A-I; 0.0016 (95% CI, 0.0009-0.0023) for lipoprotein(a); and 0.0018 (95% CI, 0.0010-0.0026) for lipoprotein-associated phospholipase A2 mass. Net reclassification improvements were less than 1% with the addition of each of these markers to risk scores containing conventional risk factors. We estimated that for 100 000 adults aged 40 years or older, 15 436 would be initially classified at intermediate risk using conventional risk factors alone. Additional testing with a combination of apolipoprotein B and A-I would reclassify 1.1%; lipoprotein(a), 4.1%; and lipoprotein-associated phospholipase A2 mass, 2.7% of people to a 20% or higher predicted CVD risk category and, therefore, in need of statin treatment under Adult Treatment Panel III guidelines.
Conclusion
In a study of individuals without known CVD, the addition of information on the combination of apolipoprotein B and A-I, lipoprotein(a), or lipoprotein-associated phospholipase A2 mass to risk scores containing total cholesterol and HDL-C led to slight improvement in CVD prediction.
JAMA 2012, June 20;307:2499-2506
Background
Risk prediction scores for cardiovascular disease (CVD) contain information on total cholesterol, HDL-C and several other conventional risk factors [1,2]. Whether CVD prediction could be improved by assessing various additional lipid-related markers to replace or to supplement traditional cholesterol measurements is an interesting topic [3].Aims of this study were to determine whether replacing information on total cholesterol and HDL-C with various lipid parameters improves prediction of first-onset CVD outcomes, and secondly to determine whether additional information on apolipoprotein B and A-I, lipoprotein(a), or lipoprotein-associated phospholipase A2 to prognostic models containing information on total cholesterol, HDL-C, and other conventional risk factors improves CVD risk prediction.
Data on 165 000 individuals from 37 cohort studies where these apolipoproteins were measured at baseline were combined and the patients were followed for an average of 10 years.
Main results
- Measuring a combination of apolipoprotein B (apoB) and apoA1, lipoprotein (a) (Lp[a]), or lipoprotein-associated phospholipase A2 (Lp-PLA2) gave worse predictions of risk than current lipid measures—total and HDL cholesterol.
- Measuring these alternative biomarkers added little information when added to conventional risk factors (fig. 1 / table 1).
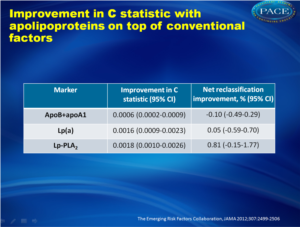 Table 1.Improvement in C statistic with apolipoproteins on top of conventional factors Click on image to enlargeSee left column to download as PowerPoint |
Conclusion
Measuring newer lipid biomarkers in addition to conventional markers only slightly improved CVD risk prediction. The clinical benefits of using newer biomarkers needs to be established.
Editorial comment [4]
The additional apolipoproteins do not add much to risk prediction over routine lipid measures. The main reason for this is probably that cardiovascular disease is multifactorial and that apolipoproteins are only one set of factors among many. A common mistake in clinical practice is to overly emphasize one or another risk factor as a predictive factor. This is particularly problematic when risk factors are colinearly linked, as occurs between lipid and apolipoprotein risk factors. The predictive power of various biomarkers does not necessarily equate to the benefit achieved by reducing them. So epidemiological studies cannot be taken as the final word, and drug therapy that targets the risk factor might still prove more efficacious than would be predicted from epidemiological studies.Recommendations for statin use in primary prevention may need to be revisited now anyway, and risk assessment may in the future move away from measuring many biomarkers and instead focus on subclinical atherosclerosis with imaging methods or simple risk projection based on age, sex, LDL levels, and perhaps another major risk factor.
References
1. Perk J, De Backer G, Gohlke H, et al. European Guidelines on cardiovascular disease prevention in clinical practice (version 2012): The Fifth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of nine societies and by invited experts) [published online May 2, 2012]. Eur Heart J2. Parish S, Offer A, Clarke R, et al. Lipids and Lipoproteins and Risk of Different Vascular Events in the MRC/BHF Heart Protection Study. Circulation. 2012;125(20):2469-2478
3. Arsenault BJ, Boekholdt SM, Kastelein JJP. Lipid parameters for measuring risk of cardiovascular disease. Nat Rev Cardiol. 2011;8(4):197-206
4. Grundy S M. Use of emerging lipoprotein risk factors in assessment of cardiovascular risk. JAMA 2012; 307:2540-2542.
Abstract
ContextThe value of assessing various emerging lipid-related markers for prediction of first cardiovascular events is debated.
Objective To determine whether adding information on apolipoprotein B and apolipoprotein A-I, lipoprotein(a), or lipoprotein-associated phospholipase A2 to total cholesterol and high-density lipoprotein cholesterol (HDL-C) improves cardiovascular disease (CVD) risk prediction.
Design, Setting, and Participants
Individual records were available for 165 544 participants without baseline CVD in 37 prospective cohorts (calendar years of recruitment: 1968-2007) with up to 15 126 incident fatal or nonfatal CVD outcomes (10 132 CHD and 4994 stroke outcomes) during a median follow-up of 10.4 years (interquartile range, 7.6-14 years).
Main Outcome Measures
Discrimination of CVD outcomes and reclassification of participants across predicted 10-year risk categories of low (<10%), intermediate (10%-<20%), and high (≥20%) risk.
Results
The addition of information on various lipid-related markers to total cholesterol, HDL-C, and other conventional risk factors yielded improvement in the model's discrimination: C-index change, 0.0006 (95% CI, 0.0002-0.0009) for the combination of apolipoprotein B and A-I; 0.0016 (95% CI, 0.0009-0.0023) for lipoprotein(a); and 0.0018 (95% CI, 0.0010-0.0026) for lipoprotein-associated phospholipase A2 mass. Net reclassification improvements were less than 1% with the addition of each of these markers to risk scores containing conventional risk factors. We estimated that for 100 000 adults aged 40 years or older, 15 436 would be initially classified at intermediate risk using conventional risk factors alone. Additional testing with a combination of apolipoprotein B and A-I would reclassify 1.1%; lipoprotein(a), 4.1%; and lipoprotein-associated phospholipase A2 mass, 2.7% of people to a 20% or higher predicted CVD risk category and, therefore, in need of statin treatment under Adult Treatment Panel III guidelines.
Conclusion
In a study of individuals without known CVD, the addition of information on the combination of apolipoprotein B and A-I, lipoprotein(a), or lipoprotein-associated phospholipase A2 mass to risk scores containing total cholesterol and HDL-C led to slight improvement in CVD prediction.
