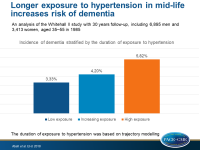
Longer exposure to hypertension in mid-life increases risk of dementia
Individuals with hypertension at mid-life, defined as SBP ≥130 mmHg at the age of 50, have an increased risk of dementia, which is proportional to the duration of the exposure to hypertension
Association between systolic blood pressure and dementia in the Whitehall II cohort study: role of age, duration, and threshold used to define hypertensionLiterature - Abell JG, Kivimaki M, Dugravot A, et al. - Eur Heart J 2018; published online ahead of print
Introduction and methods
Although lowering blood pressure (BP) in older adults does not influence the risk of dementia, data show that hypertension in mid-life is associated with an increased risk of dementia later in life [1-3]. In relevant studies however, ‘mid-life’ ranged from 35 to 68 years, hypertension was identified based on use of antihypertensive medication rather than on BP measurements, and the threshold of 140 mmHg was used for systolic BP (SBP), although lower SBP targets are required to reduce the risk of cardiovascular disease (CVD) [4,5].
The Whitehall II study is a large ongoing prospective cohort study of 6,895 men and 3,413 women, who were at age 35–55 in 1985. In this analysis of the Whitehall II study, the association between measured SBP, diastolic blood pressure (DBP) and dementia was evaluated, based on age, duration of hypertension, and SBP threshold to define hypertension. The Whitehall II study now has 30 years of follow-up. Dementia was identified using ICD-10 codes in electronic health records, while the use of medication for CVD was self-reported. The duration of exposure to hypertension was based on trajectory modelling.
Main results
- Higher SBP starting from 130 mmHg at the age of 50 was associated with an increased risk of dementia (HR: 1.38; 95%CI: 1.11-1.70). There was no association between hypertension and dementia at the age of 60 (HR: 1.03; 95%CI: 0.81-1.30) or 70 (HR: 1.14; 95%CI: 0.85-1.54).
- The use of antihypertensive medication at 50 years of age was not associated with the risk of dementia (HR: 1.16; 95%CI: 0.75-1.80). At 60 years, a significant association was seen (HR: 1.62; 95%CI: 1.21-2.18), but not at 70 years (HR: 1.32; 95%CI: 0.96-1.82).
- There was no association between DBP and incidence of dementia at age 50, 60, or 70 years.
- Three hypertension trajectories were identified, as a measure for duration of hypertension status. The incidence of dementia increased with longer exposure to SBP ≥130 mmHg , from 3.33% in participants with low exposure, to 4.20% in participants with increasing exposure, and to 5.82% in participants with high exposure (HR for low vs increasing: 1.15; 95%CI: 0.84-1.57; HR for low vs high: 1.29; 95%CI: 1.00-1.66).
- The association between hypertension at the age of 50 and dementia was not fully explained by CVD, since there was an increased risk of dementia in those without CVD (HR: 1.47; 95%CI: 1.15-1.87).
Conclusion
Individuals with hypertension at mid-life, defined as SBP ≥130 mmHg at the age of 50, have an increased risk of dementia, independently of the presence or absence of CVD. Interestingly, this association is seen below the conventional 140 mmHg threshold used to define hypertension. The risk increases with longer exposure to hypertension, but hypertension in late life is not associated with dementia risk.
References
1. Peters R, Beckett N, Forette F, et al. Incident dementia and blood pressure lowering in the Hypertension in the Very Elderly Trial cognitive function assessment (HYVET-COG): a double-blind, placebo controlled trial. Lancet Neurol 2008;7:683–689.
2. Tzourio C, Anderson C, Chapman N, et al. Effects of blood pressure lowering with perindopril and indapamide therapy on dementia and cognitive decline in patients with cerebrovascular disease. Arch Intern Med 2003;163:1069–1075.
3. Whitmer RA, Sidney S, Selby J, et al. Midlife cardiovascular risk factors and risk of dementia in late life. Neurology 2005;64:277–281.
4. Weber MA, Schiffrin EL, White WB, et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J Clin Hypertens (Greenwich) 2014;16:14–26.
5. Chobanian AV. Hypertension in 2017-what is the right target? JAMA 2017;317:579–580.