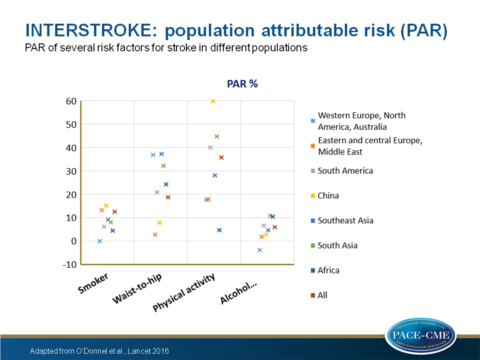
Magnitude of importance of risk factors for stroke varies between populations
Ten modifiable risk factors identified in INTERSTROKE phase I are applicable to different patient subgroups and geographic populations, but their impact can differ between groups.
Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control studyLiterature - O’Donnell et al., Lancet 2016
MJ O’Donnell, SL Chin, S Rangarajan, et al.
Lancet 2016;doi:10.1016/S0140-6736(16)30506-2
Background
Phase I of the INTERSTROKE study (n=6000, 22 countries) identified 10 potential modifiable risk factors that were associated with 90% of the population attributable risk (PAR) of acute ischemic stroke and intracerebral haemorrhage (1). However, the population was too small to reliably describe regional variations in the effect of risk factors, as well as within key populations or within stroke pathological subtypes. Nevertheless, it is important to know whether stroke prevention differs by region or population characteristics. Furthermore, variation between groups my explain the worldwide variation in stroke incidence and subtypes observed (2).In this second phase of the INTERSTROKE study, sample size was increased to 13,000 acute stroke and 13,000 control individuals of 32 countries. Some control individuals suffered from chronic bronchitis (3%), malaria (7%), tuberculosis (2%), venous thrombosis (0.9%) or peripheral vascular disease (0.8%). Measurement of the ten key vascular risk factors included self-reported hypertension of high blood pressure (BP) (≥140/90 mm Hg), current smoking, waist-to-hip ratio, diet, regular physical activity, self-reported history of diabetes, alcohol intake, psychosocial factors, cardiac causes and apolipoprotein (Apo) B/ApoA1 ratio. Variation between world regions, stroke subtypes and other patient characteristics were examined and related to the ten risk factors.
Main results
- 77.3% of patients had ischaemic stroke, 22.7% had intracerebral haemorrhage.
- Associated with all stroke were a history of hypertension or high BP, regular physical activity, apolipoprotein (Apo) B/ApoA1 ratio, diet, waist-to-hip ratio, psychosocial factors, current smoking, cardiac causes, alcohol consumption and diabetes mellitus (DM). This was similar for ischaemic stroke.
- Associated with intracerebral haemorrhage were a history of hypertension of high BP, regular physical activity, diet, waist-to-hip ratio, psychosocial factors, cardiac causes and alcohol consumption.
- Combining all ten risk factors, PAR was 90.7% (88.7-92.4) for all stroke, 91.5% (89.4-93.2) for ischaemic stroke and 87.1% (82.2-90.8) for intracerebral haemorrhage.
- In all regions an association of hypertension was seen with all stroke and of ApoB/ApoA1 ratio and atrial fibrillation with ischaemic stroke.
- Variable between regions was the association of smoking to all stroke (PAR 4.5% in Africa vs 18% in western Europe, North America and Australia), of waist-to-hip ratio to all stroke (lowest in eastern and central Europe, Middle East and China, highest in western Europe, North America, Australia, south Asia and southeast Asia), of physical inactivity to all stroke (ranged from 4.7% in Africa to 59.9% in China) and of alcohol intake to all stroke (lowest in Western Europe, North America and Australia, and highest in Africa and south Asia).
- Increasing mAHEI (modified alternative healthy eating index) score was associated with an increased risk of stroke in south Asia. However, daily intake of fruit and vegetables was associated with reduced odds in all regions but not for south Asia and Africa.
- Between men and women, the composite PAR of all ten risk factors was 90.6% for both. However PAR for smoking and alcohol consumption was greater among men than women (smoking 16.6 and 5.3%, alcohol 10 and -0.7% respectively) because of higher prevalence, whereas waist-to-hip ratio and cardiac causes were associated with a larger odds ratio in women than in men.
- People older than 55 yrs corresponded to a composite PAR of 90.0% and younger than 55 yrs to 92.2%. Younger age (<55yrs) was associated with greater odds for hypertension, waist-to-hip ratio and cardiac risk factors. On the other hand, diet had a greater influence on stroke in older (>55 yrs) individuals.
Conclusion
Despite differences in the magnitude of importance regarding risk factors between ethnic variations, men and women and age-related subgroups, the collective contribution of the ten risk factors for stroke risk was consistent in all populations (PAR ~90% for stroke). This means that general approaches for stroke prevention can be similar worldwide, but population-specific refinement of programmes might be needed.Find this article online at The Lancet
Editorial comment (3)
The associated editorial comment of Feigin strengthens the importance of the findings by O’Donnel et al.. Feigin mentions three key messages that can be drawn from the study: 1. Stroke is a highly preventable disease regardless of age and sex, 2. The relative importance of modifiable risk factors and their PAR strengthens the need for development of regional or ethnic-specific prevention programmes, 3. Additional research for risk factors is needed for countries and ethnic groups that have not been included in this analysis, as well as definite cost-effectiveness research on primary stroke prevention in key populations. ‘The key issues now are how best to implement primary prevention strategies in practice and how to decide who will provide funding for the development and implementation of integrative preventative programmes as well as research on primary prevention.’References
1. O’Donnell MJ, Xavier D, Liu L, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet 2010; 376: 112–23.
2. Feigin VL, Krishnamurthi RV, Parmar P, et al. Update on the global burden of ischemic and hemorrhagic stroke in 1990−2013: the GBD 2013 Study. Neuroepidemiology 2015; 45: 161−76.
3. Feigin VL, Krishnamurthi R. Stroke is largely preventable across the globe: where to next? Lancet. 2016:doi;10.1016/S0140-6736(16)30679-1.
