Normal glucose regulation in prediabetes associated with reduced risk for disease progression
11/06/2012
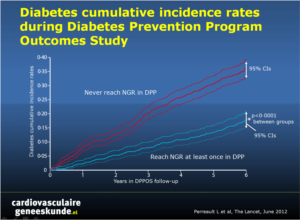
In the Diabetes Prevention Program Outcomes Study (DPPOS) long-term diabetes risk reduction was established in participants who achieved normal glucose regulation. Reaching normal glucose regulation could reduce the risk of incident diabetes significantly and durable compared with participants with persistent prediabetes.
Effect of regression from prediabetes to normal glucose regulation on long-term reduction in diabetes risk: results from the Diabetes Prevention Program Outcomes StudyLiterature - Perreault L et al; Lancet June 9 2012
Leigh Perreault, Qing Pan, Kieren J Mather, et al, for the Diabetes Prevention Program Research Group
Lancet 2012 (published online before print) DOI:10.1016/S0140-6736(12)60525-X
Background
Prediabetes is a collective term for impaired fasting glucose or impaired glucose tolerance (or both). Screening for prediabetes is advised, as it is an important risk factor for future type 2 diabetes and can cause diabetic complications [1-4]. Prevention of diabetes and its complications may result in the reversal of prediabetes and the restoration of normal glucose regulation.The Diabetes Prevention Program (DPP) examined predictors for the restoration of normal glucose regulation [5]. After completion, the Diabetes Prevention Program Outcomes Study (DPPOS) was initiated, giving the opportunity to establish the perseverance of predictors of normal glucose regulation (treatment-related or otherwise) and to quantify long-term diabetes risk reduction in participants who achieved normal glucose regulation. It was hypothesized that reaching normal glucose regulation could reduce the risk of incident diabetes significantly and durable compared with participants with persistent prediabetes. In this analysis, 1990 participants of DPPOS were included.
Main results
- Participants who achieved normal glucose regulation status at least once during DPP had a 56% reduced risk of progression to diabetes during DPPOS (HR 0.44, 95% CI 0.37-0.55, p<0.0001); risk reduction was strongly associated with the number of times normal glucose regulation was achieved
- Risk reduction was unaffected by previous group assignment
- Factors associated with an increased risk for diabetes were inversely related to the likelihood of a patient reaching normal glucose regulation. These included previous achievement of normal glucose regulation (OR=3.18; 95% CI, 2.71-3.72), insulin sensitivity (OR=3.18; 95% CI, 2.71-3.72) and increased beta-cell function (OR=1.28; 95% CI, 1.18-1.39) were associated with normal glucose regulation
Conclusion
Aggressive glucose-lowering treatments aimed at achieving normal glucose levels in people with prediabetes achieve maximum reductions in progression to diabetes in the long-term
Editorial comment [6]
The findings suggest regression of poor glucose tolerance to normoglycemia to be either spontaneous or in response to treatment. Factors that predict regression to normoglycemia, what makes this regression temporary or sustained, and whether regression reduces long-term outcomes are all questions that need further research. The results of such research might substantially change the therapeutic strategy from diabetes prevention and lifelong glucose-lowering treatment to induction of regression and monitoring use for relapse.
References
1. Diabetes Prevention Program Research Group. The prevalence of retinopathy in impaired glucose tolerance and recent-onset diabetes in the Diabetes Prevention Program. Diabet Med 2007;24:137–44.2. Cheng YJ, Gregg EW, Geiss LS, et al. Association of A1C and fasting plasma glucose levels with diabetic retinopathy prevalence in the U.S. population: implications for diabetes diagnostic thresholds. Diabetes Care 2009;32:2027–32.
3. Ford ES, Zhao G, Li C. Pre-diabetes and the risk for cardiovascular disease: a systematic review of the evidence. J Am Coll Cardiol 2010;55:1310–17.
4. Ziegler D, Rathmann W, Dickhaus T, Meisinger C, Mielck A. Prevalence of polyneuropathy in pre-diabetes and diabetes is associated with abdominal obesity and macroangiopathy: the MONICA/KORA Augsburg Surveys S2 and S3. Diabetes Care 2008;31:464–69.
5. Perreault L, Kahn SE, Christophi CA, Knowler WC, Hamman RF. Regression from pre-diabetes to normal glucose regulation in the Diabetes Prevention Program. Diabetes Care 2009;32:1583–88.
6. Yakubovich N, erstein HG. Is regression to normoglycaemia clinically important? Lancet 2012 (published online before print) DOI:10.1016/S0140-6736(12)60828-9
Abstract
Background:Our objective was to quantify and predict diabetes risk reduction during the Diabetes Prevention Program Outcomes Study (DPPOS) in participants who returned to normal glucose regulation at least once during the Diabetes Prevention Program (DPP) compared with those who consistently met criteria for prediabetes.
Methods:
DPPOS is an ongoing observational study of participants from the DPP randomised trial. For this analysis, diabetes cumulative incidence in DPPOS was calculated for participants with normal glucose regulation or prediabetes status during DPP with and without stratification by previous randomised treatment group. Cox proportional hazards modelling and generalised linear mixed models were used to quantify the effect of previous (DPP) glycaemic status on risk of later (DPPOS) diabetes and normal glucose regulation status, respectively, per SD in change. Included in this analysis were 1990 participants of DPPOS who had been randomly assigned to treatment groups during DPP (736 intensive lifestyle intervention, 647 metformin, 607 placebo).
Findings:
Diabetes risk during DPPOS was 56% lower for participants who had returned to normal glucose regulation versus those who consistently had prediabetes (hazard ratio [HR] 0•44, 95% CI 0•37—0•55, p<0•0001) and was unaffected by previous group assignment (interaction test for normal glucose regulation and lifestyle intervention, p=0•1722; normal glucose regulation and metformin, p=0•3304). Many, but not all, of the variables that increased diabetes risk were inversely associated with the chance of a participant reaching normal glucose regulation status in DPPOS. Specifically, previous achievement of normal glucose regulation (odds ratio [OR] 3•18, 95% CI 2•71—3•72, p<0•0001), increased β-cell function (OR 1•28; 95% CI 1•18—1•39, p<0•0001), and insulin sensitivity (OR 1•16, 95% CI 1•08—1•25, p<0•0001) were associated with normal glucose regulation in DPPOS, whereas the opposite was true for prediction of diabetes, with increased β-cell function (HR 0•80, 95% CI 0•71—0•89, p<0•0001) and insulin sensitivity (HR 0•83, 95% CI 0•74—0•94, p=0•0001) having a protective effect. Among participants who did not return to normal glucose regulation in DPP, those assigned to the intensive lifestyle intervention had a higher diabetes risk (HR 1•31, 95% CI 1•03—1•68, p=0•0304) and lower chance of normal glucose regulation (OR 0•59, 95% CI 0•42—0•82, p=0•0014) than did the placebo group in DPPOS.
Interpretation:
We conclude that prediabetes is a high-risk state for diabetes, especially in patients who remain with prediabetes despite intensive lifestyle intervention. Reversion to normal glucose regulation, even if transient, is associated with a significantly reduced risk of future diabetes independent of previous treatment group.