On-statin HDL-c and apoA-I levels strongly and inversely correlated with risk of CV events
These associations are largely independent of achieved LDL-c levels. Increase of apoA-I on statins is associated with a lower CV risk, while no such effect is seen for HDL-c changes.
Levels and Changes of HDL Cholesterol and Apolipoprotein A-I in Relation to Risk of Cardiovascular Events among Statin-Treated Patients: A Meta-AnalysisLiterature - Boekholdt SM, Arsenault BJ, Hovingh GK, et al. - Circulation. 2013. doi:10.1161/CIRCULATIONAHA.113.002670
Boekholdt SM, Arsenault BJ, Hovingh GK, et al.
Circulation. 2013. doi:10.1161/CIRCULATIONAHA.113.002670
Background
Both low levels of HDL-c and apolipoprotein A-I (apoA-I) are considered risk factors for coronary heart disease (CHD) [1,2]. HDL-c was found to be inversely associated with risk of cardiovascular events among people with low LDL-c levels [3], and HDL-c is still an important risk factor for patients treated with statins [4,5].Although HDL-c and apoA-I have become adopted as important therapeutic targets, their direct biological protection against atherosclerosis or risk of CHD has never been proven. In fact, several lines of evidence question HDL-c and apoA-I as relevant therapeutic targets, since raising HDL-c might not be related to a lower risk of CHD [6,7]. Also it has been suggested that changes in HDL-c after initiation of lipid-modifying therapy are not independently associated with CHD risk [8,9]. Trials testing HDL-c raising therapies have shown lack of efficacy [10] or even excess mortality in the CETP inhibitor arm [11,12].
This study therefore tested the hypothesis that higher levels of HDL-c and apoA-I are associated with lower CV risk in statin-treated patients, even in those achieving very low LDL-c levels. The authors performed a meta-analysis of individual patient data from 8 large statin trials.
Main results
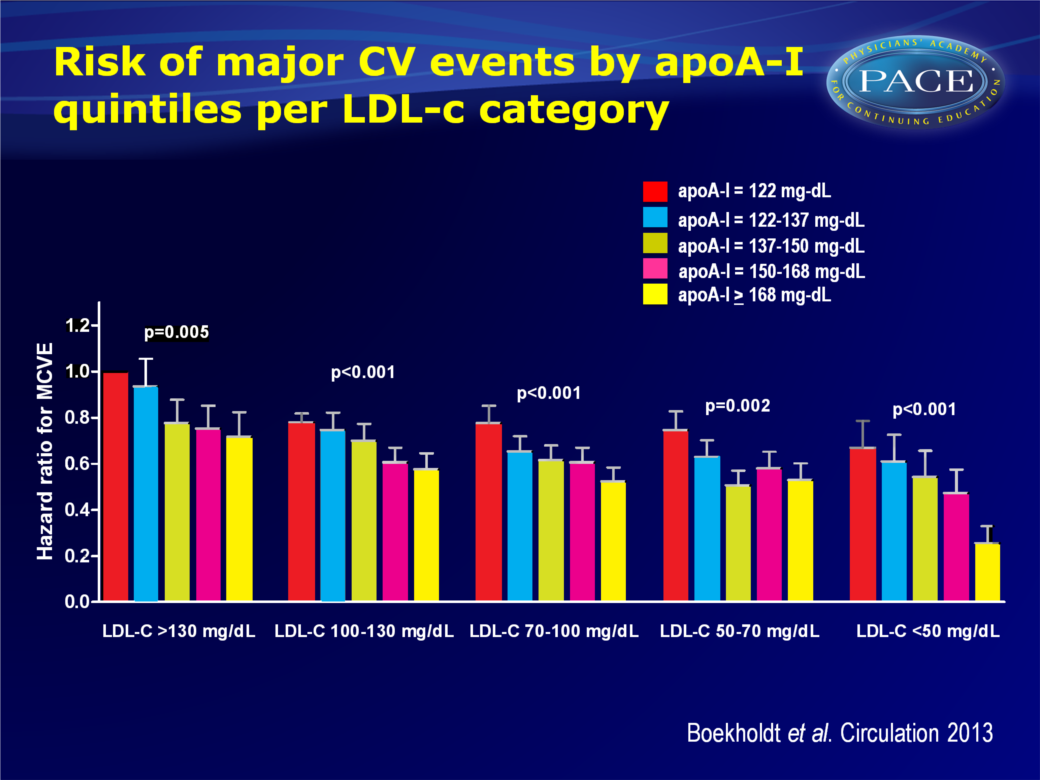
- Risk of major CV events was inversely associated with on-statin levels of HDL-c and apoA-I. Patients in the top quintile of on-statin HDL-c had an adjHR of 0.65 (95%CI: 0.59-0.71) as compared to those in the bottom quintile (P for linear trend across quintiles: <0.001).
Patients in the top quintile of on-statin apoA-I had an adjHR of 0.53 (95%CI: 0.48-0.59, P(linear trend)<0.001) as compared to those in the bottom quintile. - The association between on-statin HDL-c levels and risk of major CV events did not differ much between subgroups of patients achieving different levels of on-statin LDL-c.
- Statistically significant correlations were seen between baseline HDL-c and change in HDL-c (correlation coefficient: -0.198, P<0.001) and baseline apoA-I and change in apoA-I (corr.coef: -0.312, P<0.001).
- No large differences in risk of major CV events were seen between patients in the highest quintile of HDL-c change, as compared to patients in the lowest quintile.
Patients in the top quintile of apoA-I change had a HR 0.83 (95%C(: 0.74-0.93) as compared to patients in the lowest quintile (P for trend: 0.001).
Click on image to download
Conclusion
Among statin-treated patients, on-trial HDL-c and apoA-I are both strongly and inversely correlated with the risk of CV events, even when very low LDL-c levels have been achieved. When apoA-I levels increase after patients have started taking statins, they have a lower risk of CV events as compared to patients in whom apoA-I levels decreased. No such difference for HDL-c change after initiation of statin therapy was seen. Thus, a rise in HDL-c levels is not independently associated with a lower risk of major CV events. Modifying apoA-I levels as a preventive therapy is worth further exploration.References
1. Wilson PW, Garrison RJ, Castelli WP, et al. Prevalence of coronary heart disease in the Framingham Offspring Study: role of lipoprotein cholesterols. Am J Cardiol. 1980;46:649-654.
2. Emerging Risk Factors Collaboration. Major lipids, apolipoproteins, and risk of vascular
disease. JAMA. 2009;302:1993-2000.
3. deGoma EM, Leeper NJ, Heidenreich PA. Clinical significance of high-density lipoprotein cholesterol in patients with low low-density lipoprotein cholesterol. J Am Coll Cardiol. 2008;51:49-55.
4. Sacks FM, Tonkin AM, Shepherd J, et al. Effect of pravastatin on coronary disease events in
subgroups defined by coronary risk factors: the Prospective Pravastatin Pooling Project. Circulation. 2000;102:1893-1900.
5. Barter P, Gotto AM, LaRosa JC, et al. HDL cholesterol, very low levels of LDL cholesterol, and cardiovascular events. N Engl J Med. 2007;357:1301-1310.
6. Voight BF, Peloso GM, Orho-Melander M, et al. Plasma HDL cholesterol and risk of myocardial infarction: a mendelian randomisation study. Lancet. 2012;380:572-580.
7. Ridker PM, Genest J, Boekholdt SM, et al; JUPITER Trial Study Group. HDL cholesterol and residual risk of first cardiovascular events after treatment with potent statin therapy: an analysis from the JUPITER trial. Lancet. 2010;376:333-339.
8. Ray K, Wainwright NW, Visser L, et al. Changes in HDL cholesterol and cardiovascular outcomes after lipid modification therapy. Heart. 2012;98:780-785.
9. Briel M, Ferreira-Gonzalez I, You JJ, et al. Association between change in high density lipoprotein cholesterol and cardiovascular disease morbidity and mortality: systematic review and meta-regression analysis. BMJ. 2009;338:b92.
10. AIM-HIGH Investigators. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med. 2011;365:2255-2267.
11. Barter PJ, Caulfield M, Eriksson M, et al; ILLUMINATE Investigators. Effects of torcetrapib in patients at high risk for coronary events. N Engl J Med. 2007;357:2109-2122.
12. Schwartz GG, Olsson AG, Abt M, et al; dal-OUTCOMES Investigators. Effects of dalcetrapib in patients with a recent acute coronary syndrome. N Engl J Med. 2012;367:2089-2099.
