Patients’ perception of treatment burden greatly affects net benefit of lowering HbA1c
If moderate control of HbA1c level (9%) is achieved, a patient’s view of treatment burden is the most important factor determining the net benefit of glucose-lowering treatment.
Effect of patients' risks and preferences on health gains with plasma glucose level lowering in type 2 diabetes mellitusLiterature - Vijan S et al., JAMA Intern Med. 2014 - JAMA Intern Med. 2014 Aug 1;174(8):1227-34
VijanS, Sussman JB, Yudkin JS, et al.
JAMA Intern Med. 2014 Aug 1;174(8):1227-34. doi: 10.1001/jamainternmed.2014.2894
Background
Lowering HbA1c level delays the onset and slows progression of early microvascular disease in patients with type 2 diabetes (T2DM) [1,2]. However, trials have not found that 10 years of improved glycaemic control leads to significant reductions in clinically relevant end points such as vision loss, end-stage renal disease and amputation [1].If treatments have limited or delayed benefits, the burden and risk of treatment become more important, as they may have a negative impact on patient quality of life. Guidelines therefore recommend that patient preferences, age, and health status be taken into account when glucose management targets are set for patients with T2DM [3-5]. This is however difficult to put into practice, as there is a lack of quantitative estimation of the benefits and burdens of treating various HbA1c levels with different glycaemic medications.
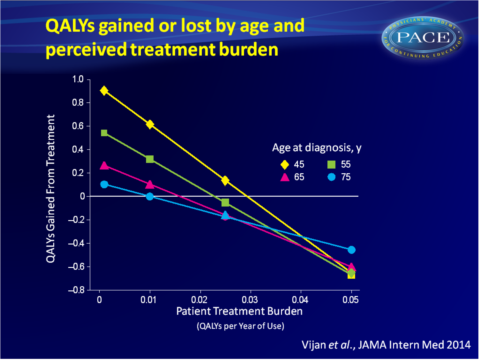
This study aimed to quantify the advantages of using a tailored approach for intensifying glycaemic control and to examine thresholds at which treatment decisions become sensitive to the level of treatment burden (quantified as ‘disutility’: a small loss in quality of life). Using a Markov simulation model, effects of HbA1c reduction on diabetes outcomes and overall quality-adjusted life years (QALYs) were estimated. Simulated patients were based on adult T2DM patients drawn from the National Health and Nutrition Examination Study (NHANES).
Main results
- In a best-case scenario (improving HbA1c lowers CHD event risk, minimal treatment burden), substantial benefits were seen, particularly among younger individuals. Reduction of HbA1c from 8.5% to 7.5% yields a gain of 0.906 QALYs in a person of 45-year old, while at 65 years it is only 0.269 QALYs and at 75 years only 0.104 QALYs gained.
- Patient perception of treatment burden profoundly impacts the net benefit of HbA1c lowering. Even when treatment improves glycaemic control by 1%, the model predicts a loss of 0.653 and 0.818 QALYs when treatment burden is high at 0.05 (equivalent to 18.2 days of high-quality lost per year, a level often reported by people receiving insulin).
- Two representative treatment scenarios were examined. Starting with metformin, with a relatively small treatment disutility, produces benefits across the whole age spectrum (ranging from 0.148 QALYs in a 75-year-old to 1.2 QALYs in a 45-year-old). Modelling starting with insulin after 10 years of oral agents however, yields a negative effect on QALYs across all age groups: the adverse effects and burdens of treatment outweigh the benefits of better glycaemic control.
Download Vijan JAMA 2014 PACE.pptx
Conclusion
In a simulation model, it was found that once moderate control of HbA1c level (9%) was achieved, a patient’s view of treatment burden is the most important factor determining the net benefit of glucose-lowering treatment. Age at diagnosis also greatly affects the net treatment benefit, with a noteworthy extent to which older patients experience smaller benefits from glycaemic control. Thus, not only HbA1c level targets need to be individualised, but individualised treatment decisions based on patients’ preferences and views on the treatment burden are at least as important.Find this article on Pubmed
References
1. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352(9131):837-853.
2. ACCORD Study Group; ACCORD Eye Study Group; Chew EY, AmbrosiusWT, Davis MD, et al. Effects of medical therapies on retinopathy progression in type 2 diabetes. N Engl J Med. 2010; 363(3):233-244.
3. American Diabetes Association. Standards of medical care in diabetes—2013. Diabetes Care. 2013;36(suppl 1):S11-S66.
46. American Geriatrics Society. Choosing wisely: five things physicians and patients should question. 2013. http://americangeriatrics.org/health_care _professionals/clinical_practice/clinical_guidelines _recommendations/choosingwisely. Accessed November 7, 2013.
5. Ismail-Beigi F, Moghissi E, Tiktin M, Hirsch IB, Inzucchi SE, Genuth S. Individualizing glycemic targets in type 2 diabetes mellitus: implications of recent clinical trials. Ann Intern Med. 2011;154(8): 554-559.
