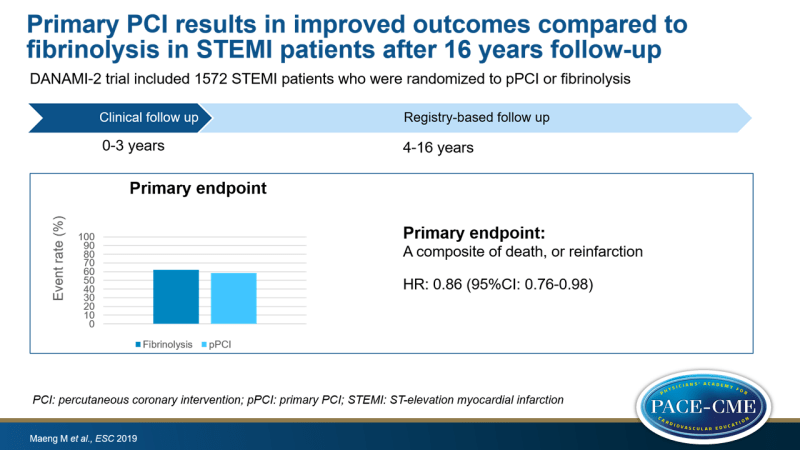
Primary PCI results in improved outcomes compared to fibrinolysis in STEMI patients after 16 years follow-up
ESC 2019 16-year follow-up of the DANAMI-2 trial showed that primary PCI lowered composite of death and reinfarction in STEMI patients compared to fibrinolysis.
16-year follow-up of the DANish Acute Myocardial Infarction 2 trial DANAMI-2News - Sep. 2, 2019
Presented at the ESC congress 2019 in Paris, France by: Michael Maeng (Aarhus, Denmark)
Introduction and methods
Landmark trials in the 1990s, such as Zwolle and PAMI, have demonstrated primary PCI (pPCI) treatment is superior to fibrinolysis in patients admitted to invasive centers. Later, in 2003, the DANAMI-2 trial showed pPCI with inter-hospital transport to invasive centers is superior to fibrinolysis after 30 days follow-up.
The current analysis of the DANAMI-2 trial includes data of 16 year follow-up.
In the DANAMI-2 trial, 1572 STEMI patients were included and randomized to pPCI or fibrinolysis in invasive centers (n=443) or in referral hospitals and subsequently transported to invasive centers (n=1129). The main endpoint of this analysis was a composite of death, or reinfarction. Data from year 4-16 was obtained from registries in Denmark.
Main results
- The composite endpoint occurred in 62.3% of patients in the fibrinolysis group and 58.7% in the pPCI group, an absolute difference of 3.6% (HR: 0.86, 95%CI:0.76-0.98, P=0.022).
- Mean gain in time to first event was 12.3 months (95%CI: 5.0-19.5).
- Individual endpoint of reinfarction and cardiac death were reduced in the pPCI group compared to the fibrinolysis group (for reinfarction: 24.5% with fibrinolysis vs. 19.0% with pPCI, HR: 0.75, 95%CI:0.60-0.93, P=0.008 and for cardiac death: 22.7% with fibrinolysis vs. 18.3% with pPCI, HR:0.78, 95%CI: 0.63-0.98, P=0.035).
- All-cause death was not different between the two groups.
- Results were similar when only patients from referral hospitals were included.
Conclusion
At 16 years follow-up, primary PCI reduced the composite endpoint of death or reinfarction in STEMI patients compared to fibrinolysis. Primary PCI extended time to first even with one year. The investigators concluded that physicians should feel confident that primary PCI is the best option to treat STEMI patients if transport to an invasive centers can be achieved within two hours.
Discussion
All-cause death was not reduced with pPCI compared to fibrinolysis, but this can be explained by competing risk. The average age at 16 years follow-up was 78 years; by that time people die from other causes.
Maeng emphasized that it is important that patients have to be transported within two hours after diagnosis. Under these conditions, pPCI is the best approach. A better option is of course to bypass the local hospital to prevent delay.
In response to the question what can explain the difference between pPCI and fibrinolysis, Maeng said that after a first diagnosis 80% appears to have definite STEMI. When pPCI is considered and patients do not appear to have definite STEMI physicians further look into the diagnosis. This is not happening when fibrinolysis is given.
- Our reporting is based on the information provided at the ESC congress -