RAAS inhibitors and mortality reduction
02/05/2012
This meta-analysis evaluated the impact of RAAS inhibitors for the indication hypertension on all-cause and cardiovascular mortality. ACE inhibitors and ARBs were studied separately as well.
Angiotensin-converting enzyme inhibitors reduce mortality in hypertension: a meta-analysis of randomized clinical trials of renin-angiotensin-aldosterone system inhibitors involving 158 998 patients.Literature - van Vark LC et al Eur Heart J. 2012 Apr 17
van Vark LC, Bertrand M, Akkerhuis KM, et al.
Eur Heart J. 2012 Apr 17.
Hypertension treatment should aim at reducing the long-term risk of (cardiovascular) morbidity and mortality [1,2]. Blockade of the RAAS is an important target, as an overactive RAAS is strongly associated with high blood pressure. Currently, the most clinically relevant pharmacological agents that block the RAAS are angiotensin-converting enzyme (ACE) inhibitors and AT1 receptor blockers (ARBs). This meta-analysis evaluated the impact of RAAS inhibitors for the indication hypertension on all-cause and cardiovascular mortality. ACE inhibitors and ARBs were studied separately as well.
158.998 patients were included in the cohort in 20 trials.
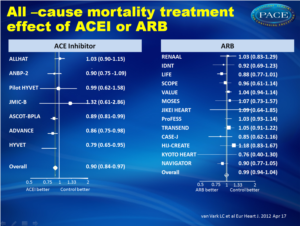
Treatment with a RAAS inhibitor was associated with a 5% reduction in all-cause mortality (HR: 0.95, 95% CI: 0.91-1.00, P=0.032). Overall reduction in cardiovascular mortality was 7% (HR:0.93, 95% CI: 0.88-0.99, P=0.018). ACE inhibitors were associated with a 10% reduction in all-cause mortality (IR: 20.4 vs 24.2 deaths/1000 patient years; HR: 0.90, 95% CI: 0.,84-0.97, P=0.004); with ARB treatment, mortality reduction was not significant (IR: 21.4 vs 22.0 deaths/1000 patient years; HR: 0.99, 95% CI: 0.94-1.04, P=0.683).
This analysis had some limitations. There was a great deal of variation between the studied populations, which can make it more difficult to accurately estimate the effect of RAAS inhibition in a broad range of daily clinical practice situations.
The analysis is based on trial data, not on individual patient data, making it difficult to judge on background therapy and co-morbidities; the follow-up time was not always available and therefore sometimes estimated, maybe causing under- or overestimation of mortality incidence. The analysis assumes a class effect among ACE inhibitors and ARBs, which might not be valid; differences may exist between drugs within the same class that are missed due to lack of statistical power.
1. Ezzati M, Lopez AD, Rodgers A, et al. Comparative Risk Assessment Collaborating G. Selected major risk factors and global and regional burden of disease. Lancet 2002;360:1347–1360.
2. Mancia G, De Backer G, Dominiczak A, et al. Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2007;28: 1462–1536.
Renin-angiotensin-aldosterone system (RAAS) inhibitors are well established for the reduction in cardiovascular morbidity, but their impact on all-cause mortality in hypertensive patients is uncertain. Our objective was to analyse the effects of RAAS inhibitors as a class of drugs, as well as of angiotensin-converting enzyme (ACE) inhibitors and AT1 receptor blockers (ARBs) separately, on all-cause mortality.
Methods and results
We performed a pooled analysis of 20 cardiovascular morbidity-mortality trials. In each trial at least two-thirds of the patients had to be diagnosed with hypertension, according to the trial-specific definition, and randomized to treatment with an RAAS inhibitor or control treatment. The cohort included 158 998 patients (71 401 RAAS inhibitor; 87 597 control). The incidence of all-cause death was 20.9 and 23.3 per 1000 patient-years in patients randomized to RAAS inhibition and controls, respectively. Overall, RAAS inhibition was associated with a 5% reduction in all-cause mortality (HR: 0.95, 95% CI: 0.91-1.00, P= 0.032), and a 7% reduction in cardiovascular mortality (HR: 0.93, 95% CI: 0.88-0.99, P= 0.018). The observed treatment effect resulted entirely from the class of ACE inhibitors, which were associated with a significant 10% reduction in all-cause mortality (HR: 0.90, 95% CI: 0.84-0.97, P= 0.004), whereas no mortality reduction could be demonstrated with ARB treatment (HR: 0.99, 95% CI: 0.94-1.04, P= 0.683). This difference in treatment effect between ACE inhibitors and ARBs on all-cause mortality was statistically significant (P-value for heterogeneity 0.036).
Conclusion
In patients with hypertension, treatment with an ACE inhibitor results in a significant further reduction in all-cause mortality. Because of the high prevalence of hypertension, the widespread use of ACE inhibitors may result in an important gain in lives saved.
Eur Heart J. 2012 Apr 17.
Background
Hypertension treatment should aim at reducing the long-term risk of (cardiovascular) morbidity and mortality [1,2]. Blockade of the RAAS is an important target, as an overactive RAAS is strongly associated with high blood pressure. Currently, the most clinically relevant pharmacological agents that block the RAAS are angiotensin-converting enzyme (ACE) inhibitors and AT1 receptor blockers (ARBs). This meta-analysis evaluated the impact of RAAS inhibitors for the indication hypertension on all-cause and cardiovascular mortality. ACE inhibitors and ARBs were studied separately as well.158.998 patients were included in the cohort in 20 trials.
Main results
Treatment with a RAAS inhibitor was associated with a 5% reduction in all-cause mortality (HR: 0.95, 95% CI: 0.91-1.00, P=0.032). Overall reduction in cardiovascular mortality was 7% (HR:0.93, 95% CI: 0.88-0.99, P=0.018). ACE inhibitors were associated with a 10% reduction in all-cause mortality (IR: 20.4 vs 24.2 deaths/1000 patient years; HR: 0.90, 95% CI: 0.,84-0.97, P=0.004); with ARB treatment, mortality reduction was not significant (IR: 21.4 vs 22.0 deaths/1000 patient years; HR: 0.99, 95% CI: 0.94-1.04, P=0.683).Conclusion
RAAS inhibitors reduce all-cause mortality in patients with hypertension. The effect results almost completely from the class of ACE-inhibitors. Widespread use of ACE inhibitors may result in a considerable gain in lives saved.
Note
This analysis had some limitations. There was a great deal of variation between the studied populations, which can make it more difficult to accurately estimate the effect of RAAS inhibition in a broad range of daily clinical practice situations.The analysis is based on trial data, not on individual patient data, making it difficult to judge on background therapy and co-morbidities; the follow-up time was not always available and therefore sometimes estimated, maybe causing under- or overestimation of mortality incidence. The analysis assumes a class effect among ACE inhibitors and ARBs, which might not be valid; differences may exist between drugs within the same class that are missed due to lack of statistical power.
References
1. Ezzati M, Lopez AD, Rodgers A, et al. Comparative Risk Assessment Collaborating G. Selected major risk factors and global and regional burden of disease. Lancet 2002;360:1347–1360.2. Mancia G, De Backer G, Dominiczak A, et al. Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2007;28: 1462–1536.
Abstract
AimsRenin-angiotensin-aldosterone system (RAAS) inhibitors are well established for the reduction in cardiovascular morbidity, but their impact on all-cause mortality in hypertensive patients is uncertain. Our objective was to analyse the effects of RAAS inhibitors as a class of drugs, as well as of angiotensin-converting enzyme (ACE) inhibitors and AT1 receptor blockers (ARBs) separately, on all-cause mortality.
Methods and results
We performed a pooled analysis of 20 cardiovascular morbidity-mortality trials. In each trial at least two-thirds of the patients had to be diagnosed with hypertension, according to the trial-specific definition, and randomized to treatment with an RAAS inhibitor or control treatment. The cohort included 158 998 patients (71 401 RAAS inhibitor; 87 597 control). The incidence of all-cause death was 20.9 and 23.3 per 1000 patient-years in patients randomized to RAAS inhibition and controls, respectively. Overall, RAAS inhibition was associated with a 5% reduction in all-cause mortality (HR: 0.95, 95% CI: 0.91-1.00, P= 0.032), and a 7% reduction in cardiovascular mortality (HR: 0.93, 95% CI: 0.88-0.99, P= 0.018). The observed treatment effect resulted entirely from the class of ACE inhibitors, which were associated with a significant 10% reduction in all-cause mortality (HR: 0.90, 95% CI: 0.84-0.97, P= 0.004), whereas no mortality reduction could be demonstrated with ARB treatment (HR: 0.99, 95% CI: 0.94-1.04, P= 0.683). This difference in treatment effect between ACE inhibitors and ARBs on all-cause mortality was statistically significant (P-value for heterogeneity 0.036).
Conclusion
In patients with hypertension, treatment with an ACE inhibitor results in a significant further reduction in all-cause mortality. Because of the high prevalence of hypertension, the widespread use of ACE inhibitors may result in an important gain in lives saved.