Renal and cardiovascular protective effects of ARBs potentiated by dietary sodium moderation
The goal of this study was to investigate if a low-sodium diet (= low urinary sodium excretion) increases the efficacy of an ARB on hard renal and cardiovascular end points in type 2 diabetic patients with nephropathy.
Renal and cardiovascular protective effects of ARBs potentiated by dietary sodium moderationLiterature - Lambers Heerspink HJ et al, Kidney Int doi:10.1038/ki.2012.74
Kidney Int doi:10.1038/ki.2012.74
Background
Agents interfering with the renin-angiotensin-aldosterone system (RAASi) are considered a cornerstone in the prevention of end-stage renal and cardiovascular disease in patients with diabetes, both early and late stage [1-4]. To further optimize the efficacy of RAASi, dietary sodium restriction might be useful, as this might enhance the response of both blood pressure and albuminuria to ARBs in diabetic and nondiabetic patients with chronic kidney disease [5,6].The goal of this study was to investigate if a low-sodium diet (= low urinary sodium excretion) increases the efficacy of an ARB on hard renal and cardiovascular end points in type 2 diabetic patients with nephropathy. Therefore, data of the Reduction of Endpoints in NIDDM with the Angiotensin II Antagonist Losartan (RENAAL) and Irbesartan Diabetic Nephropathy Trial (IDNT) trials were merged and analyzed.
Main results
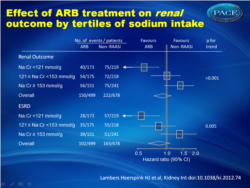
Long-term effects on renal and cardiovascular events were biggest in the lowest tertile of sodium intake with ARB therapy compared to non-RAASi-therapy. The effects on renal and cardiovascular events attenuated in subjects with higher sodium consumption; in the highest tertile the protective effects were completely offset. In the lowest tertile, a trend toward greater relative risk reductions for hospitalization for heart failure events was observed.Conclusion
Moderately low dietary sodium intake enhances the effect of RAAS intervention on renal and CV outcome. These data support calls for population-wide intervention to reduce dietary salt intake, not only for its beneficial effect on renal/CV morbidity/mortality, but also for its beneficial effect on therapy response to RAAS intervention
Author’s comment
The results of this study demonstrate unequivocally that salt reduction is essential for protection against heart disease and progression of kidney damage in patients dependent on RAAS blockade. Moreover, the study shows that the beneficial effect already occurs with only mild salt restriction, which corresponds to recent results from short term studies and in patients with non-diabetic kidney disease. These results demonstrate the importance of lifestyle correction in addition to optimal pharmacological treatment. Based on these results, in the future many health benefits may be expected.
References
1. Brenner BM, Cooper ME, de Zeeuw D et al. Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med 2001; 345: 861–869.
2. Lewis EJ, Hunsicker LG, Clarke WR et al. Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med 2001; 345: 851–860.
3. Parving HH, Lehnert H, Brochner-Mortensen J et al. The effect of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetes. N Engl J Med 2001; 345: 870–878.
4. Lambers Heerspink HJ, Ninomiya T, Perkovic V et al. Effects of a fixed combination of perindopril and indapamide in patients with type 2 diabetes and chronic kidney disease. Eur Heart J 2010; 31: 2888–2896.
5. Ekinci EI, Thomas G, Thomas D et al. Effects of salt supplementation on the albuminuric response to telmisartan with or without hydrochlorothiazide therapy in hypertensive patients with type 2 diabetes are modulated by habitual dietary salt intake. Diabetes Care 2009; 32: 1398–1403.
6. Vogt L, Waanders F, Boomsma F et al. Effects of dietary sodium and hydrochlorothiazide on the antiproteinuric efficacy of losartan. J Am Soc Nephrol 2008; 19: 999–1007.