Renal denervation effectively reduces ambulatory blood pressure
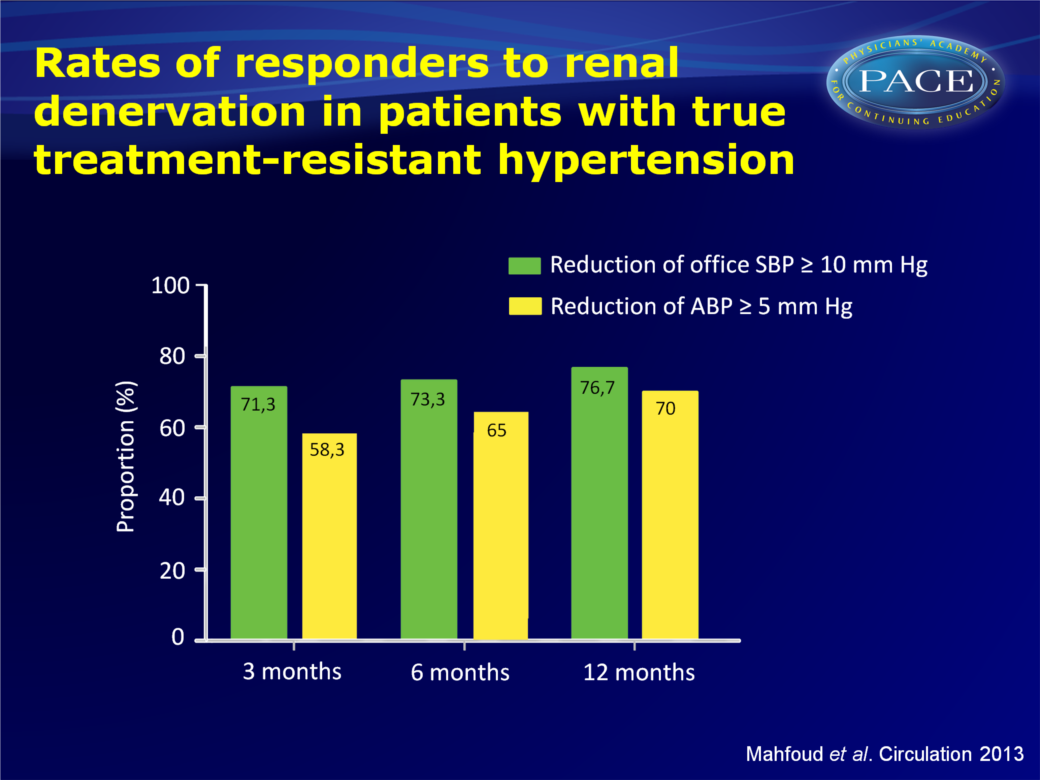
RDN reduced office and ABP in patients with true treatment-resistant hypertension, at 3, 6 and 12 months.
Ambulatory Blood Pressure Changes after Renal Sympathetic Denervation in Patients with Resistant Hypertension.Literature - Mahfoud F, Ukena C, Schmieder RE et al. - Circulation. 2013 Jun 18
Mahfoud F, Ukena C, Schmieder RE et al.
Circulation. 2013 Jun 18. [Epub ahead of print]
Background
Ambulatory blood pressure monitoring (ABPM) is recommended by international guidelines in patients with resistant hypertension to exclude pseudo-resistance and to more accurately assess the effect of treatment on BP control [1]. ABPM with 24-hour, day and night average BP values correlate better with hypertensive or diabetic end-organ damage than office BP values [2-4]. Furthermore, nighttime BP is more closely related to cardiovascular morbidity and mortality than daytime BP [5,6].Catheter-based renal denervation (RDN) reduces renal and total body norepinephrine spillover [7-9]. It lowers office systolic and diastolic BP in patients with resistant hypertension [10,11], but only limited information on its effects on daytime, night-time and average BP are available, from the Symplicity HTN-2 trial [10]. This study investigated out-of-office BP by 24-hour ABPM after RDN in a large cohort of patients with true resistant and pseudo resistant hypertension.
Main results
- Despite antihypertensive treatment, baseline SBP and DBP were 170.7+22.1 mmHg, and 91.3+15.2 mmHg respectively. Office and 24-hour mean SBP at baseline were 172.2+22 and 154+16.2 mmHg in true resistant hypertension, and 161.2+20.3 and 121.1+19.6 mmHg in pseudo-resistant hypertension.
- Office-based BP were significantly reduced in the overall cohort at 3, 6 and 12 months (SBP: -21.5/-23.7/-27.3 mmHg, DBP: -8.9/-9.5/-11.7 mmHg, n=245/236/90 for 3/6/12 months, P<0.001 for all). 24-hour SBP was reduced by 8.4/8.7/9.9 mmHg and DBP by 4.2/4.3/6.6 mmHg after 3, 6 and 12 months.
- Office BP reductions were similar in treatment resistant and pseudo-resistant hypertensive patients. 24-hour mean SBP and DBP were only significantly reduced after 3, 6 and 12 months in patients who were truly treatment resistant.
- In a subgroup of patients treated with an aldosterone antagonist (n=78), RDN lowered office SBP/DBP (-29.0/-11.4 mmHg, P<0.001 for all) and 24-hour SBP/DBP (-11.9/-7.1 mmHg, P<0.001) 6 months after RDN.
- Response to RDN was defined as SBP reduction >10 mmHg in office-based measurement and >5 mmHg in ABPM. Office SBP at baseline was identified as a correlate of response at 6 months follow-up (per 1 mmHg: OR: 1.026, 95%CI: 1.005-1.048, P=0.017, office SBP>170 mmHg: OR: 2.32: 95%CI: 1.09-4.85, P=0.029).
Conclusion
This study contradicts recent concerns that RDN might not reduce ABP equally effective as office BP. RDN significantly reduced office and 24-hour average, daytime and night-time BP in patients with true treatment-resistant hypertension. Longer-term studies should investigate the impact of these alterations on cardiovascular outcome in patients with resistant hypertension.Editorial comment [12]
Initial studies on the efficacy of RDN in lowering BP had not excluded the possibility of pseudoresistance, as the focus was on conventional office BP. The current paper offers for the first time data on ambulatory BP changes after RDN. The observed 24h ABP reduction relative to the reduction in office BP was lower than that the ratio seen for other antihypertensive therapies. This means that the degree of ambulatory BP reduction is less impressive than that of office BP. Reduction of night-time BP was similar to that of daytime BP. Consequently, no improvement was seen in altered (nondipper or reverse dipper) circadian BP profiles. Since studies have shown that nocturnal BP may be more closely related to outcome than is daytime BP, it is reassuring that night-time BP is effectively reduced by RDN.The study has several limitations thus the matter requires further study. At the same time it emphasises the importance of out-of-office BP to properly assess the effects of RDN on hypertension control in daily life.
Referenties
1. Mancia G, De Backer G, Dominiczak A, et al. 2007 guidelines for the management of arterial hypertension: The task force for the management of arterial hypertension of the european society of hypertension (esh) and of the european society of cardiology (esc). J Hypertens. 2007;25:1105-1187.
2. Mancia G, Parati G. Ambulatory blood pressure monitoring and organ damage. Hypertension. 2000;36:894-900.
3. Mancia G, Zanchetti A, Agabiti-Rosei E, et al. Ambulatory blood pressure is superior to clinic blood pressure in predicting treatment-induced regression of left ventricular hypertrophy. Sample study group. Study on ambulatory monitoring of blood pressure and lisinopril evaluation. Circulation. 1997;95:1464-1470.
4. Jula A, Puukka P, Karanko H. Multiple clinic and home blood pressure measurements versus ambulatory blood pressure monitoring. Hypertension. 1999;34:261-266.
5. Fagard RH, Celis H, Thijs L, et al. Daytime and nighttime blood pressure as predictors of death and cause-specific cardiovascular events in hypertension. Hypertension. 2008;51:55-61.
6. Metoki H, Ohkubo T, Kikuya M, Asayama et al. Prognostic significance for stroke of a morning pressor surge and a nocturnal blood pressure decline: The ohasama study. Hypertension. 2006;47:149-154.
7. Krum H, Schlaich M, Whitbourn R, et al. Catheter-based renal sympathetic denervation for resistant hypertension: A multicentre safety and proof-of-principle cohort study. Lancet.2009;373:1275-1281.
8. Krum H, Sobotka P, Mahfoud F, et al. Device-based antihypertensive therapy: Therapeutic modulation of the autonomic nervous system. Circulation. 2011;123:209-215.
9. Schlaich MP, Sobotka PA, Krum H, et al. Renal sympathetic-nerve ablation for uncontrolled hypertension. N Engl J Med. 2009;361:932-934.
10. Esler MD, Krum H, Sobotka PA, et al. Renal sympathetic denervation in patients with treatment-resistant hypertension (the symplicity htn-2 trial): A randomised controlled trial. Lancet. 2010;376:1903-1909.
11. Krum H, Barman N, Schlaich M, et al. Catheter-based renal sympathetic denervation for resistant hypertension: Durability of blood pressure reduction out to 24 months. Hypertension. 2011;57:911-917.
12. Renal Sympathetic Denervation and Daily Life Blood Pressure in Resistant Hypertension: Simplicity or Complexity? Parati G, Ochoa JE, Bilo G. Circulatio. June 18, 2013. doi: 10.1161/CIRCULATIONAHA.113.003892
