Residual risk in secondary prevention of CVD
This analysis of the Treating to New Targets (TNT) trial aimed to identify determinants of residual risk above and beyond lipid-related risk factors among patients with stable coronary disease treated to low LDL-cholesterol targets.
Determinants of Residual Risk in Secondary Prevention Patients Treated With High- Versus Low-Dose Statin Therapy: The Treating to New Targets (TNT) Study.Literature - Mora S, Enger NK, et al., Circulation. 2012;125(16):1979-87
Circulation. 2012;125(16):1979-87
Background
Cardiovascular risk remains high among statin-treated patients [1,2]. The mechanisms underlying this residual risk are unclear.This analysis of the Treating to New Targets (TNT) trial aimed to identify determinants of residual risk above and beyond lipid-related risk factors among patients with stable coronary disease treated to low LDL-cholesterol targets.
Main results
- With the use of forward stepwise regression, statistically significant variables were added to the basic model (randomization treatment, age, sex, smoking, diabetes mellitus, and hypertension).
- Multivariable determinants of increased risk were older age, increased body mass index, male sex, hypertension, diabetes mellitus, baseline apolipoprotein B and blood urea nitrogen, current smoking, prior cardiovascular disease, and calcium channel blocker use.
- Determinants of decreased risk were high-dose statin, aspirin use, and baseline apolipoprotein A-I.
- Nown baseline variables moderately discriminated future cases from noncases.
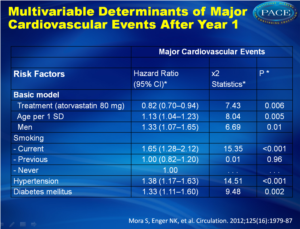 Multivariable Determinants of Major Cardiovascular Events After Year 1Click on image to enlarge See left column to download as PowerPoint |
Conclusion
A multifaceted secondary prevention approach targeting modifiable risk factors is the cornerstone of optimal residual risk assessment and prevention.
Editorial comment [3]
“TNT investigators have provided useful insights into the challenges that confront those who seek to reduce residual risk in the patient with chronic coronary disease. To achieve the potential benefits of high-dose statin therapy, the patient and his or her health professional need to focus more strongly on drug adherence, and this should be part of the risk communication when statins are prescribed. To guide prevention efforts, we need coordinated research investigations that lead to feasible policies to better recognize and manage those high-risk individuals who develop intolerance to statin therapy.To make notable progress against residual risk, a final wish is for a resource commitment so that smoking cessation and improvement in metabolic syndrome risk factor management by lifestyle can occur with higher success rates than are currently attained.”
References
1. Baigent C, Keech A, et al. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005;366:1267–1278.
2. Baigent C, Blackwell L, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376:1670–1681.
3. Stone NJ. Reducing residual risk in secondary prevention of cardiovascular disease. Circulation. 2012;125(16):1958-60.
Abstract
Background:Cardiovascular events occur among statin-treated patients, albeit at lower rates. Risk factors for this "residual risk" have not been studied comprehensively. We aimed to identify determinants of this risk above and beyond lipid-related risk factors.
Methods and results:
A total of 9251 coronary patients with low-density lipoprotein cholesterol <130 mg/dL randomized to double-blind atorvastatin 10 or 80 mg/d in the Treating to New Targets (TNT) study had complete on-treatment 1-year lipid data. Median follow-up was 4.9 years. The primary end point was major cardiovascular events (n=729): coronary death, nonfatal myocardial infarction, resuscitation after cardiac arrest, or fatal or nonfatal stroke. Multivariable determinants of increased risk were older age (adjusted hazard ratio [aHR], 1.13 per 1 SD [8.8 years]; 95% confidence interval [CI], 1.04-1.23), increased body mass index (aHR, 1.09; 95% CI, 1.02-1.17 per 4.5 kg/m(2)), male sex (aHR, 1.33; 95% CI, 1.07-1.65), hypertension (aHR, 1.38; 95% CI, 1.17-1.63), diabetes mellitus (aHR, 1.33; 95% CI, 1.11-1.60), baseline apolipoprotein B (aHR, 1.19; 95% CI, 1.11-1.28 per 19 mg/dL), and blood urea nitrogen (aHR, 1.10; 95% CI, 1.03-1.17 per 4.9 mg/dL), in addition to current smoking, prior cardiovascular disease, and calcium channel blocker use. Determinants of decreased risk were high-dose statin (aHR, 0.82; 95% CI, 0.70-0.94), aspirin use (aHR, 0.67; 95% CI, 0.56-0.81), and baseline apolipoprotein A-I (aHR, 0.91; 95% CI, 0.84-0.99 per 25 mg/dL). On-treatment 1-year lipids or apolipoproteins were not additionally associated with risk in multivariable models. Known baseline variables performed moderately well in discriminating future cases from noncases (Harrell c index=0.679).
Conclusions:
Determinants of residual risk in statin-treated secondary prevention patients included lipid-related and nonlipid factors such as baseline apolipoproteins, increased body mass index, smoking, hypertension, and diabetes mellitus. A multifaceted prevention approach should be underscored to address this risk.
