Statins appear renoprotective in subjects with CVD, with or without chronic kidney disease
eGFR improved within a year of atorvastatin treatment in subjects with known coronary heart disease, and during up to 6 years of follow-up. Diabetic patients also have renal benefit.
Effect of High-Dose Atorvastatin on Renal Function in Subjects With Stroke or Transient Ischemic Attack in the SPARCL TrialLiterature - Amarenco P et al., Stroke. 2014 - Stroke. 2014 Aug 21
AmarencoP, Callahan A, Campese VM 3rd, et al.
Stroke. 2014 Aug 21. pii: STROKEAHA.114.005832. [Epub ahead of print]
Background
To reduce the cardiovascular disease (CVD) risk associated with chronic kidney disease (CKD) and to prevent progressive impairment of renal function, aggressive treatment of comorbid conditions is recommended [1-3]. It has been shown that higher LDL-c levels are associated with a more rapid decrease in estimated glomerular filtration rate (eGFR) [4,5] and lowering LDL-c with statins may be renoprotective in subjects with CVD [6,7]. Several trials have shown improvements in eGFR with statin treatment, both in subjects with or without CKD [8-12].In the Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) trial, patients with recent noncardioembolic stroke or transient ischaemic attack (TIA) without known coronary heart disease (CHD) were randomised to atorvastatin 80 mg/d or placebo. Treatment was associated with lower stroke risk and major coronary events [13]. This paper describes a post hoc analysis of SPARCL data that explored the effect of atorvastatin 80 mg/d vs. placebo on changes in renal function from baseline (eGFR) in those with (n=1600) and without (eGFR >60 mL/min per 1.73m2, n=3119) CKD at baseline. Subjects with CKD had a baseline eGFR of 52.3±7.0 mL/min per 1.73 m2 compared with an eGFR of 72.3±8.9 mL/min per 1.73 m2 in those without CKD (P<0.001).
Main results
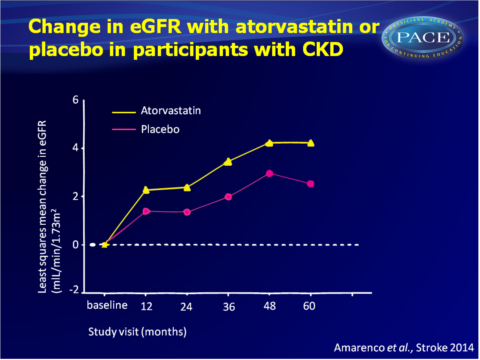
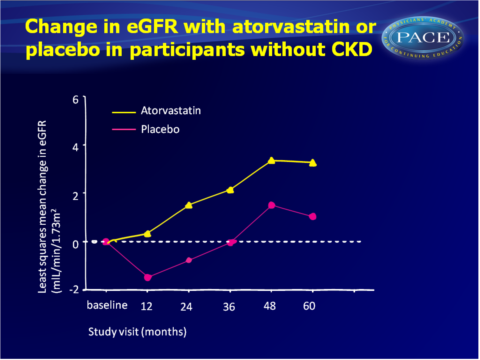
- After 60 months of treatment with atorvastatin, eGFR increased with 3.46+0.33 as compared with 1.42+0.34 mL/min per 1.73m2 in the placebo group. Improvements with atorvastatin vs. placebo were seen after 12, 24, 36, 48 and 60 months of therapy. No significant treatment by time interaction was seen.
- The improvement of eGFR with statin treatment did not depend on baseline renal function: at 60 months, atorvastatin-treated subjects with CKD showed a least squares mean rise in eGFR of 4.24+0.60 mL/min per 1.73m2, whereas those without CKD had a 3.27+0.40 mL/min per 1.73m2 increase. An improvement of eGFR was also seen in patients with placebo, but the rise was significantly larger in patients on atorvastatin.
- In subjects without CKD at baseline, fewer individuals on atorvastatin had a decline in kidney function to eGFR<60 mL/min during the trial than those assigned to placebo (10.6% vs. 14.1%, P=0.005). A greater proportion of atorvastatin-treated individuals had better kidney function at the end of the study as compared with placebo (34.1% vs. 29.3%, P=0.050).
- In patients with diabetes mellitus at randomisation, patients on placebo showed a decline in eGFR during the study (-1.69+0.92 mL/min per 1.73m2), while patients on atorvastatin showed a 1.12+0.92 mL/min per 1.73 m2 increase (P=0.016).
- Persistent elevations in hepatic transaminase levels occurred more often in atorvastatin-treated subjects than in placebo, but overall rates were low, and similar between those with (2.4%) and without (2.0%) CKD. Persistent elevations in creatine phosphokinase levels were also similar between subjects with and without CKD.
Download Amarenco STROKE 2014 PACE.pptx
Conclusion
This posthoc analysis suggests that treatment with atorvastatin 80 mg/d improves eGFR as compared with placebo, in a population of subjects with prior stroke or TIA. The decline in renal function seen in subjects who had diabetes at baseline, was largely halted in subjects randomised to atorvastatin. The renoprotective effects of atorvastatin 80 mg/d were seen within 1 year, and maintained for 60 months, and were seen in patient with and without CKD at baseline.Find this article on Pubmed
References
1. National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39:S1–S266.
2. Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int Suppl. 2013;3:1–150.
3. Wanner C, Tonelli M, The Kidney Disease: Improving Global Outcomes Lipid Guideline Development Work Group Members. KDIGO Clinical Practice Guideline for lipid management in CKD: summary of recommendation statements and clinical approach to the patient. Kidney Int. 2014;85:1303–1309.
4. Schaeffner ES, Kurth T, Curhan GC, Glynn RJ, Rexrode KM, Baigent C, et al. Cholesterol and the risk of renal dysfunction in apparently healthy men. J Am Soc Nephrol. 2003;14:2084–2091.
5. Appel GB, Radhakrishnan J, Avram MM, DeFronzo RA, Escobar- Jimenez F, Campos MM, et al; RENAAL Study. Analysis of metabolic parameters as predictors of risk in the RENAAL study. Diabetes Care. 2003;26:1402–1407.
6. Bianchi S, Bigazzi R, Caiazza A, Campese VM. A controlled, prospective study of the effects of atorvastatin on proteinuria and progression of kidney disease. Am J Kidney Dis. 2003;41:565–570.
7. Fassett RG, Robertson IK, Ball MJ, Geraghty DP, Coombes JS. Effect of atorvastatin on kidney function in chronic kidney disease: a randomised double-blind placebo-controlled trial. Atherosclerosis. 2010;213:218–224.
8. Tonelli M, Moyé L, Sacks FM, Cole T, Curhan GC; Cholesterol and Recurrent Events Trial Investigators. Effect of pravastatin on loss of renal function in people with moderate chronic renal insufficiency and cardiovascular disease. J Am Soc Nephrol. 2003;14:1605–1613.
9. Tonelli M, Isles C, Craven T, Tonkin A, Pfeffer MA, Shepherd J, et al. Effect of pravastatin on rate of kidney function loss in people with or at risk for coronary disease. Circulation. 2005;112:171–178.
10. Athyros VG, Mikhailidis DP, Papageorgiou AA, Symeonidis AN, Pehlivanidis AN, Bouloukos VI, et al. The effect of statins versus untreated dyslipidaemia on renal function in patients with coronary heart disease. A subgroup analysis of the Greek atorvastatin and coronary heart disease evaluation (GREACE) study. J Clin Pathol. 2004;57:728–734.
11. Shepherd J, Kastelein JJ, Bittner V, Deedwania P, Breazna A, Dobson S, et al; Treating to New Targets Investigators. Effect of intensive lipid lowering with atorvastatin on renal function in patients with coronary heart disease: the Treating to New Targets (TNT) study. Clin J Am Soc Nephrol. 2007;2:1131–1139.
12. Koren MJ, Davidson MH, Wilson DJ, Fayyad RS, Zuckerman A, Reed DP; ALLIANCE Investigators. Focused atorvastatin therapy in managed- care patients with coronary heart disease and CKD. Am J Kidney Dis. 2009;53:741–750.
13. Amarenco P, Bogousslavsky J, Callahan A III, Goldstein LB, Hennerici M, Rudolph AE, et al; Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) Investigators. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med. 2006;355:549–559.
