Statins beneficial as primary and secondary prevention
05/03/2013
Meta-analysis evaluates the effect of statins on all-cause mortality and major coronary events
AbstractLiterature - Naci H, Brugts JJ, Fleurence R et al. - Eur J Prev Cardiol. March 2013
Comparative benefits of statins in the primary and secondary prevention of major coronary events and all-cause mortality: a network meta-analysis of placebo-controlled and active-comparator trials.
Naci H, Brugts JJ, Fleurence R et al.
Eur J Prev Cardiol. March 2013
Background
The effectiveness of statins in reducing coronary and cardiovascular events in patients with cardiovascular disease has previously been demonstrated in meta-analyses. Nowadays, statins are increasingly often prescribed in people at lower risk of cardiovascular disease [1]. However, consensus is lacking on the benefit of statins in primary prevention [2-5]. Moreover, it is unclear whether the clinical effects of individual statins are comparable, due to the nature of previous meta-analyses [6-9].The current meta-analysis combines evidence from 92 trials, both placebo-controlled and active-comparator trials. The effect of statins on major coronary events and all-cause mortality is evaluated across all populations, and as primary and secondary prevention of cardiovascular disease separately.
Main results
- Overall, in placebo-controlled studies, statin therapy was associated with a reduction in all cause mortality (OR 0.87, 95% CI 0.82–0.92) and major coronary events (OR 0.69, 95% CI 0.64–0.75).
- Secondary prevention showed a reduction in all cause mortality (OR 0.82, 95% CI 0.75–0.90) and major coronary events (OR 0.69, 95% CI 0.62–0.77), as did statin therapy as primary prevention: all-cause mortality (OR 0.91, 95% CI 0.83–0.99) and major coronary events (OR 0.69, 95% CI 0.61–0.79).
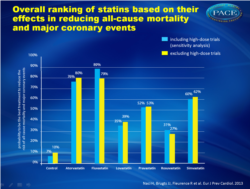
- Atorvastatin (80%), fluvastatin (79%), and simvastatin (62%) are the most effective treatments in terms of cumulative probability of reducing all-cause mortality and major coronary events across all populations, at comparable doses.
Conclusions
This meta-analysis shows an effect of 18% reduction of all cause mortality when statins are used as secondary prevention, in patients with cardiovascular disease. The effect is less, but still 9% reduction, when statins are used as primary prevention. Statins reduce the occurrence of major coronary events to a similar extent when used as primary or secondary prevention. This study provides supportive evidence for prescribing statins to high-risk individuals who have not yet developed cardiovascular disease.
References
1. Brugts JJ and Deckers JW. Statin prescription in men and women at cardiovascular risk: to whom and when?Current pinion in Cardiology 2010; 25: 484–489.
2. Minder CM, Blaha MJ, Tam LM, et al. Making the case for selective use of statins in the primary prevention setting.
Archives of Internal Medicine 2011; 171: 1593–1594.
3. Brugts JJ, Yetgin T, Hoeks SE, et al. The benefits of statins in people without established cardiovascular disease
but with cardiovascular risk factors: meta-analysis of randomised controlled trials. British Medical Journal 2009; 338: b2376.
4. Ray KK, Seshasai SR, Erqou S, et al. Statins and allcause mortality in high-risk primary prevention: a metaanalysis
of 11 randomized controlled trials involving 65,229 participants. Archives of Internal Medicine 2010; 170: 1024–1031.
5 . Taylor F, Ward K, Moore Theresa HM, et al. Statins for the primary prevention of cardiovascular disease.
Cochrane Database of Systematic Reviews 2011; (1):CD004816.
6. Mills EJ, WU P, Chong G, et al. Efficacy and safety of statin treatment for cardiovascular disease: a network
meta-analysis of 170ffl255 patients from 76 randomized trials. QJM 2011; 104: 109–124.
7. Mills EJ, Rachlis B, Wu P, et al. Primary prevention of cardiovascular mortality and events with statin treatments: a network meta-analysis involving more than 65,000 patients. Journal of American College of Cardiology 2008; 52: 1769–1781.
8. Alberton M, Wu P, Druyts E, et al. Adverse events associated with individual statin treatments for cardiovascular
disease: an indirect comparison meta-analysis. QJM 2012; 105: 145–157.
9. Zhou Z, Rahme E and Pilote L. Are statins created equal? Evidence from randomized trials of pravastatin,
simvastatin, and atorvastatin for cardiovascular disease prevention. American Heart Journal 2006; 151: 273–281.Background
The extent to which individual statins vary in terms of clinical outcomes across all populations, in addition to secondary and primary prevention has not been studied extensively in meta-analyses.
Methods
We systematically studied 199,721 participants in 92 placebo-controlled and active-comparator trials comparing atorvastatin, fluvastatin, lovastatin, pravastatin, rosuvastatin, and simvastatin in participants with, or at risk of developing, cardiovascular disease. We performed pairwise and network meta-analyses for major coronary events and all-cause mortality outcomes, taking into account the dose differences across trials. Systematic review registration: PROSPERO 2011:CRD42011001470.
Results
There were only a few trials that evaluated fluvastatin. Most frequent comparisons occurred between pravastatin and placebo, atorvastatin and placebo, and rosuvastatin and atorvastatin. No trial directly compared all six statins to each other. Across all populations, statins were significantly more effective than control in reducing all-cause mortality (OR 0.87, 95% credible interval 0.82-0.92) and major coronary events (OR 0.69, 95% CI 0.64-0.75). In terms of reducing major coronary events, atorvastatin (OR 0.66, 95% CI 0.48-0.94) and fluvastatin (OR 0.59, 95% CI 0.36-0.95) were significantly more effective than rosuvastatin at comparable doses. In participants with cardiovascular disease, statins significantly reduced deaths (OR 0.82, 95% CI 0.75-0.90) and major coronary events (OR 0.69, 95% CI 0.62-0.77). Atorvastatin was significantly more effective than pravastatin (OR 0.65, 95% CI 0.43-0.99) and simvastatin (OR 0.68, 95% CI 0.38-0.98) for secondary prevention of major coronary events. In primary prevention, statins significantly reduced deaths (OR 0.91, 95% CI 0.83-0.99) and major coronary events (OR 0.69, 95% CI 0.61-0.79) with no differences among individual statins. Across all populations, atorvastatin (80%), fluvastatin (79%), and simvastatin (62%) had the highest overall probability of being the best treatment in terms of both outcomes. Higher doses of atorvastatin and fluvastatin had the highest number of significant differences in preventing major coronary events compared with other statins. No significant heterogeneity or inconsistency was detected.
Conclusions
Statins significantly reduce the incidence of all-cause mortality and major coronary events as compared to control in both secondary and primary prevention. This analysis provides evidence for potential differences between individual statins, which are not fully explained by their low-density lipoprotein cholesterol-reducing effects. The observed differences between statins should be investigated in future prospective studies.