Statins in patients with MI and acute heart failure: results from the EPHESUS trial
24/01/2013
Jan 2013. EJHF . This study assessed the association between statin prescription at baseline and clinical outcomes in patients with acute systolic heart failure included in the EPHESUS trial.
AbstractLiterature -
Statin therapy and clinical outcomes in myocardial infarction patients complicated by acute heart failure: insights from the EPHESUS trial.
Dobre D, Rossignol P, Murin J, et al.
Eur J Heart Fail. 2013;15(2):221-7. doi: 10.1093/eurjhf/hfs128.
Background
In acute and post-acute myocardial infarction, statin therapy improves cardiovascular morbidity and mortality and all-cause mortality [1-4]. Patients with acute heart failure were however often excluded from trials [4-8]. Statin therapy may also be beneficial in initial stages of heart failure. In the EPHESUS trial(Eplerenone Post-Acute Myocardial Infarction Heart Failure Efficacy and Survival study), the effects of the mineralocorticoid receptor antagonist eplerenone were assessed in patients with acute MI complicated by clinical signs and symptoms of HF and left ventricular dysfunction [9]. About half of the patients also used a statin at baseline.This study assessed the association between statin prescription at baseline and clinical outcomes in patients with acute systolic heart failure included in the EPHESUS trial.
Main results
- During a mean follow-up of 16 ± 7 months, all-cause death occurred in 385 (12%) patients with and in 647 (18%) patients without a statin. In univariate survival analysis, the risk of all-cause death was 34% lower in statin vs. non-statin users (HR 0.66, 95% CI 0.59-0.75, P<0.001) (fig. 1).
- After extensive adjustment, the risk of all-cause death remained 20% lower in patients with vs. those without a statin (HR 0.80, 95% CI 0.69–0.92, P = 0.001), mostly due to a lower risk of CV death (HR 0.76, 95% CI 0.65–0.88, P = 0.0002). The reduction of CV death was mainly due to a lower rate of sudden death (HR 0.77, 95% CI 0.61–0.96, P = 0.02) and death from stroke (HR 0.53, 95% CI 0.28–0.96, P = 0.04), but was also due a lower rate of death from worsening HF and from recurrent acute MI.
- Statin use was associated with a higher risk of non-CV hospitalizations (HR 1.16, 95% CI 1.02–1.33, P = 0.02)
Conclusion
Patients with acute HF complicating acute MI may benefit from being on statin therapy, with a lower risk of all-cause death, mainly attributable to a lower rate of CV death.Prospective clinical trials are required to validate these findings.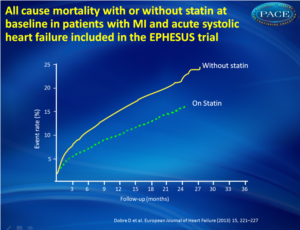 Figure 1Kaplan-Meier survival curves (all-cause death) in patients who receive or not a statin at baseline. |
References
1. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet 1994;344:1383–1389.2. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. The Long-Term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group. N Engl J Med 1998;339:1349–1357.
3. Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20,536 high-risk individuals: a randomized placebo-controlled trial. Lancet 2002;360:7–22.
4. Schwartz GG, Olsson AG, Ezekowitz MD, et al. Effects of atorvastatin on early recurrent ischemic events in acute coronary syndromes: the MIRACL study: a randomized controlled trial. JAMA 2001;285:1711–1718.
5. Cannon CP, McCabe CH, Belder R, et al. Design of the Pravastatin or Atorvastatin Evaluation and Infection Therapy (PROVE IT)-TIMI 22 trial. Am J Cardiol 2002;89:860–861.
6. Pasceri V, Patti G, Nusca A, et al. Randomized trial of atorvastatin for reduction of myocardial damage during coronary intervention:results from the ARMYDA (Atorvastatin for Reduction of Myocardial Damage during Angioplasty) study. Circulation 2004;110:674–678.
7. Patti G, Chello M, Candura D, et al. Randomized trial of atorvastatin for reduction of postoperative atrial fibrillation in patients undergoing cardiac surgery: results of the ARMYDA-3 (Atorvastatin for Reduction of MYocardial Dysrhythmia After cardiac surgery) study. Circulation 2006;114:1455–1461.
8. Pedersen TR, Faergeman O, Kastelein JJ, et al. High-dose atorvastatin vs usual-dose simvastatin for secondary prevention after myocardial infarction: the IDEAL study: a randomized controlled trial. JAMA 2005;294:2437–2445.
9. Pitt B, Remme W, Zannad F, et al. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med 2003;348:1309–1321.
Aims:
Several clinical trials have shown that in patients with acute myocardial infarction (MI), statin therapy improves cardiovascular (CV) outcomes, but in these trials patients with acute heart failure (HF) were excluded or only a few were included. In patients with chronic HF, statin therapy does not reduce all-cause or CV mortality. We aimed to assess the association between statin therapy and clinical outcomes in the setting of acute HF with systolic dysfunction complicating acute MI.
Methods and results:
We performed a post-hoc analysis in 6632 patients included in the EPHESUS trial. The mean age of patients was 64 years and 71% were male. Overall, 47% of patients had a statin prescribed at baseline. Cox regression models and a secondary analysis using propensity score matching were fit to assess the association between statin prescription and clinical outcomes. During a mean follow-up of 16 ± 7 months, all-cause death occurred in 385 (12%) patients with and in 647 (18%) patients without a statin (P < 0.001). After extensive adjustment, the risk of all-cause death was 20% lower in patients on statin [hazard ratio (HR) 0.80, 95% confidence interval (CI) 0.69-0.92, P = 0.001]. This positive association was mostly due to a lower risk of CV death (HR 0.76, 95% CI 0.65-0.88, P = 0.0002). In contrast, statin use was associated with a higher risk of non-CV hospitalizations (HR 1.16, 95% CI 1.02-1.33, P = 0.02).
Conclusion:
Our results suggest that patients with acute HF complicating acute MI may benefit from being on statin therapy. Prospective clinical trials are required to validate these findings.
