Ticagrelor in ACS and stroke
11/05/2012
This study describes the clinical efficacy and safety of ticagrelor versus clopidogrel in patients with prior stroke or TIA in a prespecified subgroup analysis of the PLATO trial.
Ticagrelor versus Clopidogrel in Patients with Acute Coronary Syndromes and a History of Stroke or Transient Ischemic AttackLiterature - James SK et al. May 9, 2012, Circulation
James SK, Storey RF, et al.
Circulation 2012, May 9 [Epub ahead of print]
Patients with ACS with a history of stroke or TIA are at high risk for recurrent cardiovascular events. For clopidogrel, it has been shown that combined with aspirin it successfully prevented thrombotic events in patients with ACS. However, patients with prior stroke continued to have a high risk of ischemic complications and bleeding complications, including an increased risk of intracranial bleeding [1,2]. In the PLATelet inhibition and patient Outcomes (PLATO) trial, ticagrelor was superior to clopidogrel for the prevention of cardiovascular death, myocardial infarction (MI) or stroke without a significant increase in overall major bleeding in a broad population of patients with ACS [3]. This study describes the clinical efficacy and safety of ticagrelor versus clopidogrel in patients with prior stroke or TIA in a prespecified subgroup analysis of the PLATO trial.
“Although statistically non-significant the reduction of ischemic endpoints with ticagrelor, however, was of the same magnitude as in patients without a prior stroke. The risk of intracranial bleeding in the studies specifically aiming for the reduction of ischemic stroke is so striking that current studies on novel dual antiplatelet therapy in ACS and thereafter exclude patients with previous stroke (also in the currently running PEGASUS trial). How will the results of the current analysis concur with the future outcome of PEGASUS? The number of patients with prior stroke in previous ACS trials is low and the number of excess intracranial bleedings by novel dual antiplatelet therapy even much lower. In case of ticagrelor the test for interaction is not statistically significant, but given the insufficient data an interaction cannot be excluded either. Routinely treating ACS patients with previous stroke or TIA with novel platelet inhibitors cannot be advised yet.”
2. Bhatt DL, Fox KA, et al. Clopidogrel and aspirin versus aspirin alone for the prevention of atherothrombotic events. N Engl J Med. 2006;354:1706-1717.
3. Wallentin L, Becker RC, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361:1045-1057.
4. Verheugt FWA. Beware of novel antiplatelet therapy in ACS patients with previous stroke. Circulation 2012 (Epub ahead of print)
Patients with acute coronary syndromes (ACS) and history of stroke or transient ischemic attack (TIA) have an increased rate of recurrent cardiac events and intracranial hemorrhages.
Methods and Results
We evaluated treatment effects of ticagrelor versus clopidogrel in ACS patients with and without a history of prior stroke or TIA in the PLATelet inhibition and patient Outcomes (PLATO) trial. Of the 18,624 randomized patients, 1,152 (6%) had history of stroke or TIA. They had higher rates of myocardial infarction (11.5 % versus 6.0 %), death (10.5 % versus 4.9 %), stroke (3.4 % versus 1.2%), and intracranial bleeding (0.8 % versus 0.2 %) when compared to patients without prior stroke or TIA. Among patients with a history of stroke or TIA the reduction of the primary composite outcome and total mortality at one year with ticagrelor vs. clopidogrel was consistent with the overall trial results: 19.0% vs. 20.8% (Hazard ratio, HR 0.87; 95% Confidence Interval, CI; 0.66-1.13, interaction p-value=0.84) and 7.9% vs. 13.0%, HR. 0.62 (95% CI; 0.42, 0.91). The overall PLATO defined bleeding rates were similar; 14.6% vs. 14.9%, HR 0.99 (95% CI; 0.71, 1.37) and intracranial bleeding occurred infrequently (4 vs. 4 cases, respectively).
Conclusions
ACS patients with prior history of ischemic stroke or TIA had higher rates of clinical outcomes when compared to patients without prior stroke and TIA. However, the efficacy and bleeding results of ticagrelor in these high risk patients were consistent with the overall trial population with a favourable clinical net benefit and associated impact on mortality.
Circulation 2012, May 9 [Epub ahead of print]
Background
Patients with ACS with a history of stroke or TIA are at high risk for recurrent cardiovascular events. For clopidogrel, it has been shown that combined with aspirin it successfully prevented thrombotic events in patients with ACS. However, patients with prior stroke continued to have a high risk of ischemic complications and bleeding complications, including an increased risk of intracranial bleeding [1,2]. In the PLATelet inhibition and patient Outcomes (PLATO) trial, ticagrelor was superior to clopidogrel for the prevention of cardiovascular death, myocardial infarction (MI) or stroke without a significant increase in overall major bleeding in a broad population of patients with ACS [3]. This study describes the clinical efficacy and safety of ticagrelor versus clopidogrel in patients with prior stroke or TIA in a prespecified subgroup analysis of the PLATO trial.
Main results
- Patients with prior stroke or TIA presented higher rates at one year of the primary composite endpoint (myocardial infarction, death, stroke, major bleeding and intracranial bleeding) when compared to those patients without prior stroke or TIA.
- The relative reduction of the primary endpoint with ticagrelor compared with clopidogrel was consistent in patients with (13%) and without (16%) prior stroke or TIA.
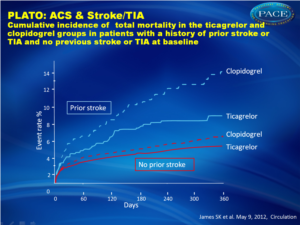
- For all-cause death, the relative reduction with ticagrelor versus clopidogrel was 38% and 19% in patients with or without a prior history of stroke, respectively (figure 1), with no significant treatment-by-stroke history interaction test.
- Among patients with a prior stroke or TIA, the rate of PLATO defined major bleeding and non CABG related major bleeding were not significantly different between patients assigned to ticagrelor and clopidogrel
Conclusion
In the subgroup of patients with a history of stroke or TIA more potent and consistent inhibition of platelet aggregation with ticagrelor reduced ischemic events with no significant increase in overall major bleeding complications, consistent with the overall PLATO trial results. The risk of intracranial haemorrhage or fatal stroke was low and total mortality was significantly reduced by ticagrelor, resulting in a favourable clinical net benefit and associated impact on mortality.
Editorial comment [4]
“Although statistically non-significant the reduction of ischemic endpoints with ticagrelor, however, was of the same magnitude as in patients without a prior stroke. The risk of intracranial bleeding in the studies specifically aiming for the reduction of ischemic stroke is so striking that current studies on novel dual antiplatelet therapy in ACS and thereafter exclude patients with previous stroke (also in the currently running PEGASUS trial). How will the results of the current analysis concur with the future outcome of PEGASUS? The number of patients with prior stroke in previous ACS trials is low and the number of excess intracranial bleedings by novel dual antiplatelet therapy even much lower. In case of ticagrelor the test for interaction is not statistically significant, but given the insufficient data an interaction cannot be excluded either. Routinely treating ACS patients with previous stroke or TIA with novel platelet inhibitors cannot be advised yet.”References
1. Yusuf S, Zhao F, et al. Clopidogrel in Unstable Angina to Prevent Recurrent Events Trial I. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without st-segment elevation. N Engl J Med.2001;345:494-502.2. Bhatt DL, Fox KA, et al. Clopidogrel and aspirin versus aspirin alone for the prevention of atherothrombotic events. N Engl J Med. 2006;354:1706-1717.
3. Wallentin L, Becker RC, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009;361:1045-1057.
4. Verheugt FWA. Beware of novel antiplatelet therapy in ACS patients with previous stroke. Circulation 2012 (Epub ahead of print)
Abstract
BackgroundPatients with acute coronary syndromes (ACS) and history of stroke or transient ischemic attack (TIA) have an increased rate of recurrent cardiac events and intracranial hemorrhages.
Methods and Results
We evaluated treatment effects of ticagrelor versus clopidogrel in ACS patients with and without a history of prior stroke or TIA in the PLATelet inhibition and patient Outcomes (PLATO) trial. Of the 18,624 randomized patients, 1,152 (6%) had history of stroke or TIA. They had higher rates of myocardial infarction (11.5 % versus 6.0 %), death (10.5 % versus 4.9 %), stroke (3.4 % versus 1.2%), and intracranial bleeding (0.8 % versus 0.2 %) when compared to patients without prior stroke or TIA. Among patients with a history of stroke or TIA the reduction of the primary composite outcome and total mortality at one year with ticagrelor vs. clopidogrel was consistent with the overall trial results: 19.0% vs. 20.8% (Hazard ratio, HR 0.87; 95% Confidence Interval, CI; 0.66-1.13, interaction p-value=0.84) and 7.9% vs. 13.0%, HR. 0.62 (95% CI; 0.42, 0.91). The overall PLATO defined bleeding rates were similar; 14.6% vs. 14.9%, HR 0.99 (95% CI; 0.71, 1.37) and intracranial bleeding occurred infrequently (4 vs. 4 cases, respectively).
Conclusions
ACS patients with prior history of ischemic stroke or TIA had higher rates of clinical outcomes when compared to patients without prior stroke and TIA. However, the efficacy and bleeding results of ticagrelor in these high risk patients were consistent with the overall trial population with a favourable clinical net benefit and associated impact on mortality.