Variability in blood pressure between visits associated with cognitive decline
In contrast to mean values, the variability in SBP and DBP between visits was associated with cognitive and verbal decline.
Visit-to-Visit Variability in Blood Pressure Is Related to Late-Life Cognitive DeclineLiterature - Qin B et al., Hypertension 2016
Qin B, Viera AJ, Munther P, et al.
Hypertension 2016;68:106-113
Background
The investigations of cognitive disorders in relation to blood pressure (BP) are commonly focussed on mean BP levels in contrast to the variability between visit-to-visit BP measurements. However, over the last 5 years evidence has accumulated that visit-to-visit BP variability may not be a random phenomenon or simply an unimportant measurement artefact, but may instead provide information on pathological processes and it can be relevant for prognosis [1,2].Although evidence demonstrated that midlife hypertension is a risk factor for cognitive decline, its association with late-life hypertension is less clear. Nor is it known whether visit-to-visit variability in BP is associated with a faster rate of cognitive decline in a general population of older adults.
Therefore, this study examined the association between visit-to-visit variability in BP and cognitive decline among a sample of community-dwelling Chinese men and women (n=976, age ≥55yrs) that were included in the China Health and Nutrition Survey (CHNS) which is an ongoing longitudinal open cohort study from 1989 onwards. In 3 waves (1997, 2000 and 2004), CHNS used identical cognitive screening items that were verified by telephone.
Main results
Systolic blood pressure (SBP)- A higher SD of SBP was associated with older age, higher urbanisation index, lower education and physical activity, having a history of stroke or diabetes mellitus, and taking antihypertensive medication.
- Mean SBP was progressively higher with increased SD of SBP (r=0.33).
- No significant association was seen between mean change in SBP and global cognitive decline (= total score of all cognitive screening items, lowest vs. highest tertile of SD of SBP, β=-0.13, P=0.09).
- The adjusted rate of global cognitive decline associated with the middle (9.30-15.00 mmHg) and highest (≥15.01 mmHg) tertile of SD of SBP was faster by -0.13 and -0.27 points per year respectively (95% CI: -0.33 to 0.06 and -0.47 to -0.07 respectively), compared to the lower tertile (<9.30 mmHg, P trend = 0.008).
For verbal memory scores this was -0.018 for the middle and -0.041 for the highest tertile of SD of SBP (95% CI: -0.051 to 0.015 respectively -0.075 to -0.008, P trend =0.02). - The associations were not dependent on age.
- Age significantly modified the association between DBP variability and cognitive decline (P=0.01).
- For those aged ≥65 yrs, a higher SD of DBP was associated with a history of myocardial infarct, but not with cognitive decline.
- Higher mean DBP and antihypertensive medication, stratified for age, were associated with increased SD of DBP (association with mean DBP r=0.14 for participants <65 yrs and 0.09 for those ≥65 yrs).
- Among adults aged <65 yrs, the adjusted rate of global cognitive decline for the middle and highest tertile of SD of SBP was faster by -0.29 respectively -0.29 points per year (95% CI: -0.53 to -0.05 for both), compared to the lower tertile (P trend = 0.02).
- There was a difference in the association between residual variation of DBP and global cognitive declines (highest vs. lowest tertile; β=-0.27, 95% CI: -0.51 to -0.03, P trend = 0.04), suggesting the relation is possibly because of the DBP fluctuation instead of the systematic pattern over time
Download Qin Hypertension 2016 PACE.pptx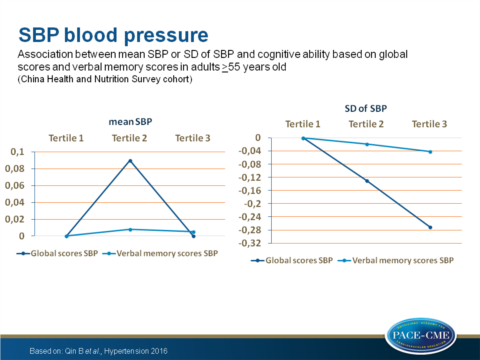
Conclusion
Higher visit-to-visit variability in SBP was associated with a faster decline of global cognitive function and to a lesser extent of verbal memory over a mean follow-up of 5 years. This was also true for DBP for adults of 55-64 years of age. In contrast, no association between mean SBP or DBP with cognitive change over time was observed.Find this article online at Hypertension
References
1. Muntner P, Joyce C, Levitan EB, Holt E, Shimbo D, Webber LS, Oparil S, Re R, Krousel-Wood M. Reproducibility of visit-to-visit variability of blood pressure measured as part of routine clinical care. J Hypertens. 2011;29:2332–2338. doi: 10.1097/HJH.0b013e32834cf213.
2. Rothwell PM, Howard SC, Dolan E, O’Brien E, Dobson JE, Dahlöf B, Sever PS, Poulter NR. Prognostic significance of visit-to-visit variability, maximum systolic blood pressure, and episodic hypertension. Lancet. 2010;375:895–905. doi: 10.1016/S0140-6736(10)60308-X
