Very low levels of atherogenic lipoproteins show CV benefit over moderately low levels
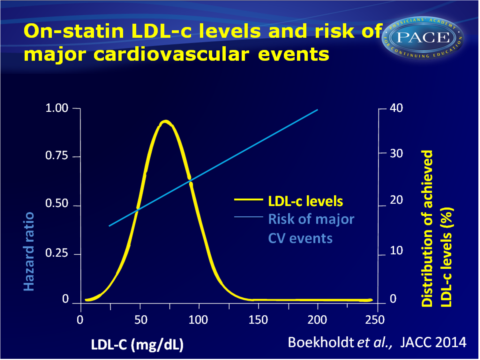
Meta-analysis shows large interindividual variation in response to high-dose statin therapy. Achieving LDL-c<50 mg/dL gives lower risk of major CV events than with LDL-c of 75-100 mg/dL.
Very Low Levels of Atherogenic Lipoproteins and the Risk for Cardiovascular Events - A Meta-Analysis of Statin TrialsLiterature - Boekholdt SM et al. JACC 2014 - J Am Coll Cardiol. 2014;64(5):485-494
Boekholdt SM, Hoving GK, Mora S et al.,
J Am Coll Cardiol. 2014;64(5):485-494. doi:10.1016/j.jacc.2014.02.615
"No clinical-outcomes trial with statins has ever achieved a mean LDL-cholesterol level much less than 70 [mg/dL]," said senior investigator Dr John Kastelein (Academic Medical Center, Amsterdam, The Netherlands). "That's why we thought it might be a good idea to get all the individual patient data and see whether we could extend the line a little further down. Of course, this is a nonrandomized, post hoc analysis, with all the caveats you should attach to it, but I think the data are very convincing."
Background
Although the efficacy of statins to reduce LDL levels and cardiovascular disease (CVD) risk is well-established, these insights are based on mean reductions in randomised trials. The extent of reduction of atherogenic lipoprotein levels varies considerably between individuals. Post-hoc analyses of randomised trials suggest that the attained LDL-c reduction may determine the benefits of statin therapy [1,2]. Furthermore, individuals who reach very low LDL-c levels, have been shown to be at very low CVD risk [3,4].Current guidelines recommend to consider 70 to 130 mg/dL as target LDL-c level. This may, however, be too conservative, when considering observational evidence. With novel lipid-lowering therapies such as mipomersen and PCSK9 inhibitors, the majority of patients may be able to reach LDL-c<70 mg/dL [5-7]. It is, however, unclear whether atherogenic lipoprotein levels in this range, obtained pharmacologically, convey CVD risk benefits.
This meta-analysis on individual patient data from 8 trials [8] therefore aimed to assess the variability of LDL-c, non-HDL-c and apoB reduction with established statin therapy, the proportion of patients not reaching target levels of these lipoproteins despite high-dose statin therapy, and how these lipoprotein levels associated with risk of major CV events.
Main results
- Waterfall plots revealed a large interindividual variation in lipoprotein reduction achieved with both initiation of usual dose and high-dose statin therapy, and in patients switched from usual to high-dose statins.
- Mean achieved LDL-c level among 18.677 patients on high-dose statin therapy was 69.6+27.0 mg/dL. 2.364 (12.7%) individuals did not reach LDL-c<100 mg/dL, while 7.546 (40.4%) did not get achieve LDL-c<70 mg/dL. 14.600 (78.3%) did not reach LDL-c<50 mg/dL.
2.176 (11.7%) did not reach non-HDL-c<130 mg/dL, and 6.285 (33.7%) did not obtain non-HDL-c below 100 mg/dL.
2.740 (14.7%) patients did not reach apoB <100 mg/dL and 6.662 (35.7%) did not achieve apoB<80 mg/dL. - Achieving LDL-c < 50 mg/dL was associated with a significantly lower risk for major CV events, as compared with those with LDL-c>175 mg/dL (adj HR: 0.44, 95%CI: 0.35-0.55).
- Also when compared with patients achieving LDL-c between 75-100 mg/dL, patients with LDL-c <50 mg/dL had a lower risk of major CV events (adj HR: 0.81, 95%CI: 0.70-0.95).
- Similarly decreasing risk with lower LDL-c levels was seen for major coronary events and major cerebrovascular events.
- Although based on low absolute numbers, the risk of haemorrhagic stroke appeared somewhat higher among patients achieving very low levels of atherogenic lipoproteins, as compared to those who reached moderately low levels.
Download Boekholdt JACC 2014 PACE.pptx
Conclusion
This meta-analysis on individual patient data shows that large interindividual variation exists in the reduction of atherogenic lipoprotein levels achieved with statin therapy. Over 40% of trial patients did not reach an LDL-c level below 70 mg/dL with high-dose statin therapy. Achieving LDL-c levels below 50 mg/dL appears, however, to confer considerable clinical benefit, as shown by the significantly lower risk of major CV events, even in comparison with patients who reach LDL-c between 75 and 100 mg/dL. Randomised controlled trials are needed to evaluate whether a strategy targeting very low levels of atherogenic lipoproteins provides clinical benefit as compared with a strategy targeting moderately low levels.Find this article online
Editorial comment [9]
‘In November 2013, the American College of Cardiology (ACC) and the American Heart Association(AHA) published a much-anticipated guideline update, in which the most surprising and controversial
change was the abandonment of LDL-C targets and dose titration. Instead, either moderate- or high intensity statin therapy was recommended on the basis of underlying risk categories, irrespective of LDL-C response.’ This meta-analysis now shows a clear relationship between LDL-C level attained and cardiovascular risk, supporting the premise that “lower is better” when it comes to LDL-C goal.
A limitation of the statin trials to date is however that they examined fixed dose statins, rather than following a strategy of individualised goal attainment. ’The main limitation, beyond the post-hoc observational nature of the data and the different inclusion criteria, which the authors acknowledged, is that the LDL-C levels attained may have been influenced by a myriad of factors, which in themselves may affect cardiovascular risk.In this regard, the present meta-analysis does not disprove the 2013 ACC/AHA guidelines contention that there are inadequate data at the present time to indicate specific LDL-C targets of therapy.’
References
1. Pedersen TR, Olsson AG, Faergeman O, et al. Lipoprotein changes and reduction in the incidence of major coronary heart disease events in the Scandinavian Simvastatin Survival Study (4S). Circulation 1998;97:1453–60.
2. Simes RJ, Marschner IC, Hunt D, et al. Relationship between lipid levels and clinical outcomes in the Long-term Intervention with Pravastatin in Ischemic Disease (LIPID) Trial: to what extent is the reduction in coronary events with pravastatin explained by on-study lipid levels? Circulation 2002;105:1162–9.
3. Wiviott SD, Cannon CP, Morrow DA, et al. Can low-density lipoprotein be too low? The safety and efficacy of achieving very low low-density lipoprotein with intensive statin therapy: a PROVE IT-TIMI 22 substudy. J Am Coll Cardiol 2005;46:1411–6.
4. Hsia J, MacFadyen JG, Monyak J, et al. Cardiovascular event reduction and adverse events among subjects attaining low-density lipoprotein cholesterol <50 mg/dl with rosuvastatin. The JUPITER trial (Justification for the Use of Statins in Prevention: an Intervention Trial Evaluating Rosuvastatin). J Am Coll Cardiol 2011; 57:1666–75.
5. Giugliano RP, Desai NR, Kohli P, et al. Efficacy, safety, and tolerability of a monoclonal antibody to proprotein convertase subtilisin/kexin type 9 in combination with a statin in patients with hypercholesterolaemia (LAPLACE-TIMI 57): a randomised, placebo-controlled, dose-ranging, phase 2 study. Lancet 2012;380:2007–17.
6. Roth EM, McKenney JM, Hanotin C, et al. Atorvastatin with or without an antibody to PCSK9 in primary hypercholesterolemia. N Engl J Med 2012;367:1891–900.
7. Thomas GS, Cromwell WC, Ali S, et al. Mipomersen, an apolipoprotein B synthesis inhibitor, reduces atherogenic lipoproteins in patients with severe hypercholesterolemia at high cardiovascular risk: a randomized double-blind placebo-controlled trial. J Am Coll Cardiol 2013;62:2178–84.
8. Boekholdt SM, Arsenault BJ, Mora S, et al. Association of LDL cholesterol, non-HDL cholesterol, and apolipoprotein B levels with risk of cardiovascular events among patients treated with statins: a meta-analysis. JAMA 2012;307: 1302–9.
9. Ben-Yehuda O, DeMaria AN. LDL-Cholesterol Targets After the ACC/AHA 2013 Guidelines. Evidence That Lower Is Better? J Am Coll Cardiol 2014;64(5):495-496
