Weight loss reduces burden and severity of atrial fibrillation
Weight reduction and improvement of multiple cardiometabolic risk factors were beneficial for cardiac structure and reduced atrial fibrillation symptom burden.
Effect of weight reduction and cardiometabolic risk factor management on symptom burden and severity in patients with atrial fibrillation: a randomized clinical trialLiterature - Abed et al., JAMA Nov 2013 - JAMA. 2013 Nov 20;310(19):2050-60
Abed HS, Wittert GA, Leong DP, et al.
JAMA. 2013 Nov 20;310(19):2050-60. doi: 10.1001/jama.2013.280521
Background
The prevalence of atrial fibrillation (AF) is predicted to rise. Population aging is generally regarded as an important contributor, but obesity may also account for a substantial proportion of the increasing prevalence [1].Obesity has been associated with several factors known to promote arrhythmogenesis [2], such as diastolic dysfunction [3], systemic proinflammatory state [4], autonomic tone abnormalities [5] and atrial enlargement [6]. Fat stores have also been shown to correlate with incident AF [7]. A direct effect of obesity was recently demonstrated on the atrial substrates [8].
This study therefore evaluated the effect of a structured weight reduction and risk factor management program on AF burden in a randomised controlled trial. 150 patients with symptomatic paroxysmal or persistent AF and BMI>27 and waist circumference greater than 100 cm in men or 90 cm in women were included. Patients were randomised to either a physician-led weight loss program or to self-directed general lifestyle measures (control group). Mean follow-up was 12.9 (95%CI: 12.3-13.5) months in the intervention group and 12.0 (95%CI: 11.1-12.9) in the control group.
Main results
- Weight, BMI and waist circumference decreased in both groups, but statistically significantly more in the intervention group. The differences were already clear by 3 months, and persisted throughout the rest of follow-up.
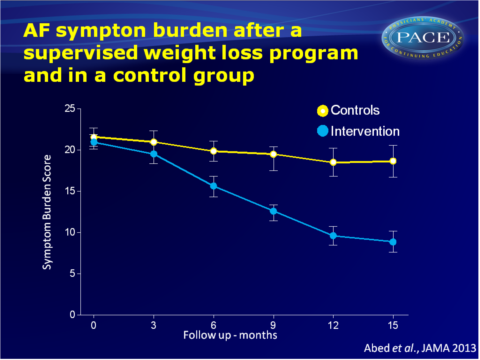
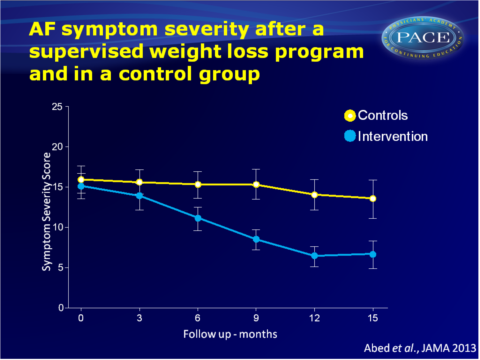
- AF symptom burden and symptom severity scores declined in both groups. No changes were seen yet in the first three months. From 6 to 15 months, the intervention group showed a greater reduction in both domains, as compared to the control group (burden score: 21.0 (95%CI: 20.1-21.9) to 8.8 (95%CI: 7.6-10.1)] vs. 21.6 (95%CI: 20.5-22.7) to 18.7 (95%CI: 16.7-20.6); symptom score, 15.2 (95% CI: 13.6-16.8) to 6.7 (95% CI: 5.0-8.4) vs. 16.0 (95%CI: 14.3-17.7).
- Holter recordings were performed at baseline and at 12 months. The mean number of AF episodes in the intervention group (n=57) decreased from 3.3 (95%CI: 1.6-4.9) to 0.62 (95%CI: 0.19-1.0) and the duration of AF decreased from 1176 (95%CI: 720-1632) minutes to 491 (95%CI: 159-822) minutes.
In the control group, the number of episodes changed from 2.8 (95%CI: 1.7-4.0) to 2.0 (95%CI: 1.1-3.0), and duration increased from 1393 (95%CI: 785-1994) minutes to 1546 (95%CI: 782-2308) minutes. - Height-indexed left atrial area and volume, and septal thickness and posterior wall thickness and height-indexed left ventricular mass decreased in all groups, but more so in the intervention group as compared to the control group.
Download Abed-obesity JAMA 2013 pace.pptx
Conclusion
This study showed that a structured weight management program for highly symptomatic patients with AF can reduce symptom burden and severity, as compared to attempts to optimally manage risk factors alone. The beneficial effects may be a consequence of a decrease in left atrial area and ventricular wall thickness, which may reduce left atrial hypertension that is commonly found in obese patients. The greater reduction in BMI in the intervention group was accompanied by improvement in other risk factors for AF.Find this article on Pubmed
References
1. Wanahita N, Messerli FH, Bangalore S, et al. Atrial fibrillation and obesity—results of ameta-analysis. Am Heart J. 2008;155(2):310-315.
2. Nattel S, Burstein B, Dobrev D. Atrial remodeling and atrial fibrillation: mechanisms and implications. Circ Arrhythm Electrophysiol. 2008;1(1):62-73.
3. Russo C, Jin Z, Homma S, et al. Effect of obesity and overweight on left ventricular diastolic function: a community-based study in an elderly cohort. J AmColl Cardiol. 2011;57(12):1368-1374.
4. VisserM, Bouter LM, McQuillan GM,et al. Elevated C-reactive protein levels in overweight and obese adults. JAMA. 1999;282(22):2131-2135.
5. Karason K, Mølgaard H,Wikstrand J, et al. Heart rate variability in obesity and the effect of weight loss. Am J Cardiol. 1999;83(8):1242-1247.
6. Stritzke J, Markus MR, Duderstadt S, et al; MONICA/KORA Investigators. The aging process of the heart: obesity is the main risk factor for left atrial enlargement during aging the MONICA/KORA (monitoring of trends and determinations in cardiovascular disease/cooperative research in the region of Augsburg) study. J AmColl Cardiol. 2009;54(21):1982-1989.
7. Wong CX, Abed HS, Molaee P, et al. Pericardial fat is associated with atrial fibrillation severity and ablation outcome. J AmColl Cardiol. 2011;57(17):1745-1751.
8. Abed HS, Samuel CS, Lau DH, et al. Obesity results in progressive atrial structural and electrical remodeling: implications for atrial fibrillation. Heart Rhythm. 2013;10(1):90-100.
